Crit Care:SARS-CoV-2相关性中重度低氧性呼吸衰竭患者早期长时间俯卧位是否能改善无创呼吸机治疗的临床结果
2022-05-13 从医路漫漫 MedSci原创
俯卧位(PP)疗法是一种非药物疗法,它通过几种机制改善氧合,包括改善通风/灌流匹配,减轻纵隔重量对依赖肺区的压迫,以及改变胸壁弹性。
背景:急性低氧性呼吸衰竭是严重急性呼吸综合征冠状病毒2型(SARS-CoV-2)感染最常见的生命威胁并发症。尽管正在进行药理学试验,但对冠状病毒病2019(新冠肺炎)肺炎和中到重度呼吸衰竭患者的治疗仍然具有支持性,这些患者中高达60%需要有创机械通气,死亡率在40%-81%之间。因此,减少这类新冠肺炎患者对有创机械通气需求的无创策略是人们热切期待的。
俯卧位(PP)疗法是一种非药物疗法,它通过几种机制改善氧合,包括改善通风/灌流匹配,减轻纵隔重量对依赖肺区的压迫,以及改变胸壁弹性。此外,PP的益处与其对气体交换的影响无关。目前,延长PP被推荐用于有侵入性呼吸机的严重急性呼吸窘迫综合征(ARDS)患者,可降低28天死亡率,但其在中至重度急性呼吸衰竭清醒患者中的作用尚不清楚。在小病例系列和观察性研究中。持续正压治疗(CPAP)可改善因SARS-CoV-2肺炎引起的不同严重程度的急性呼吸衰竭清醒患者的氧合情况,但复吸后这种效果的持久性是不稳定的,而且没有证据表明这种效果对硬结果有临床益处。
两项试验发现,在使用高流量鼻插管治疗呼吸衰竭严重程度广泛的新冠肺炎患者中,不同持续时间的清醒PP要么降低了插管率,要么没有好处。在这些试验中,接受无创呼吸机(NIV)治疗的患者没有从清醒PP中获得临床好处。因此,对不良结局风险最大的新冠肺炎患者进行非侵入性机械通气的有效性仍不确定。
目的:我们评估了早期PP对新冠肺炎肺炎致中重度急性低氧性呼吸衰竭患者28天无创机械通气失败、气管插管和死亡的影响,并探讨了治疗反应的生理机制。
方法:在这项非随机对照试验中,对2020年12月至2021年5月期间81例新冠肺炎肺炎和中重度(PaO2/FiO2<200)急性低氧性呼吸衰竭患者进行早期PP+NIV治疗,并与2020年4月至2020年12月在HUMANITAS Gradenigo亚重症监护室接受常规(仰卧式)NIV治疗的162例新冠肺炎肺炎患者进行比较,以限制混淆。分别于基线和第5天进行肺超声检查。在最初的7天内监测呼吸机参数、生理性死腔指数(DSI)以及循环炎症和促凝血生物标志物。
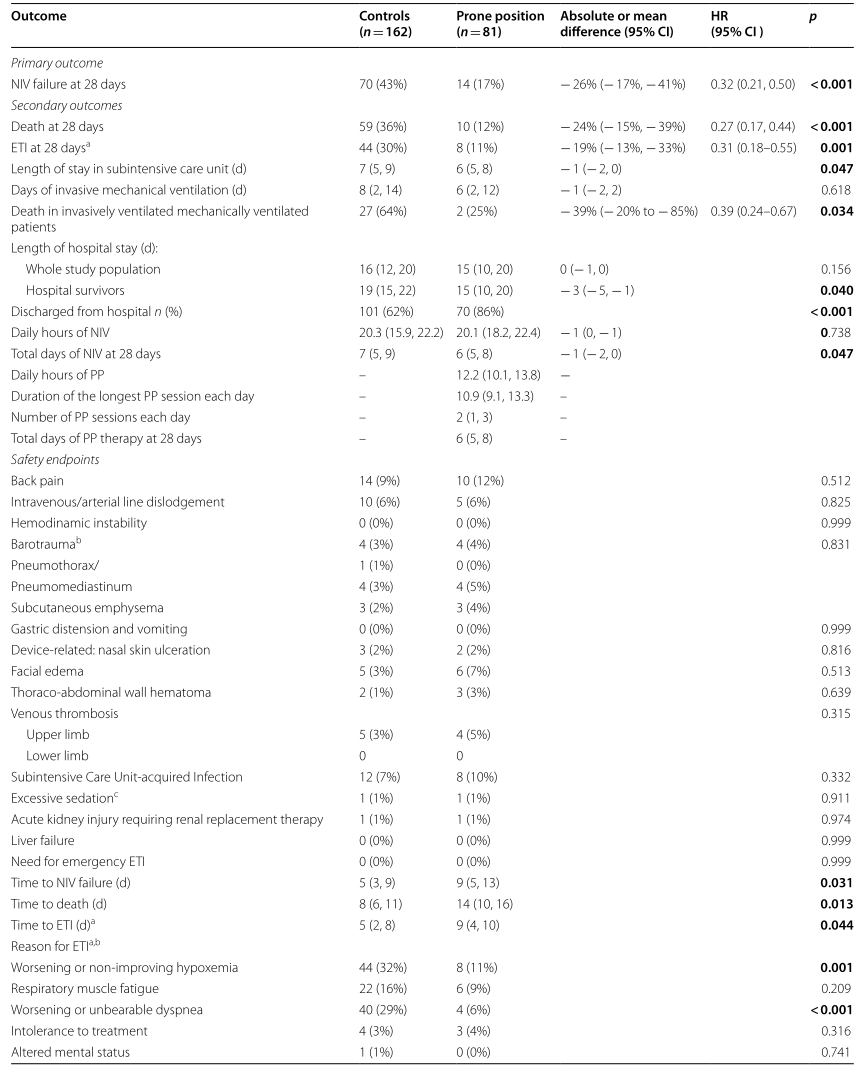
结果:在意向处理分析中。气管插管失败8例(11%),对照组44例(30%)[HR=0.31,95%CI0.18-0.55;p=0.0012];死亡10例(12%),对照组59例(36%)[HR=0.27,95%CI0.17-0.44;p<0.0001]。在不同程度的低氧血症(入院时PaO2/FiO2<100或PaO2/FiO2 100-199)中,效果仍然显著。不良反应很少见,且分布均匀。与对照组相比,PP治疗可改善氧合和DSI,通过增强肺背侧区域的复氧降低整体LUS严重指数,并提早降低炎症标志物和D-二聚体。在多变量分析中,第1天的二氧化碳反应优于氧气反应,作为LU改变、NIV失败、插管和死亡的预测因子。
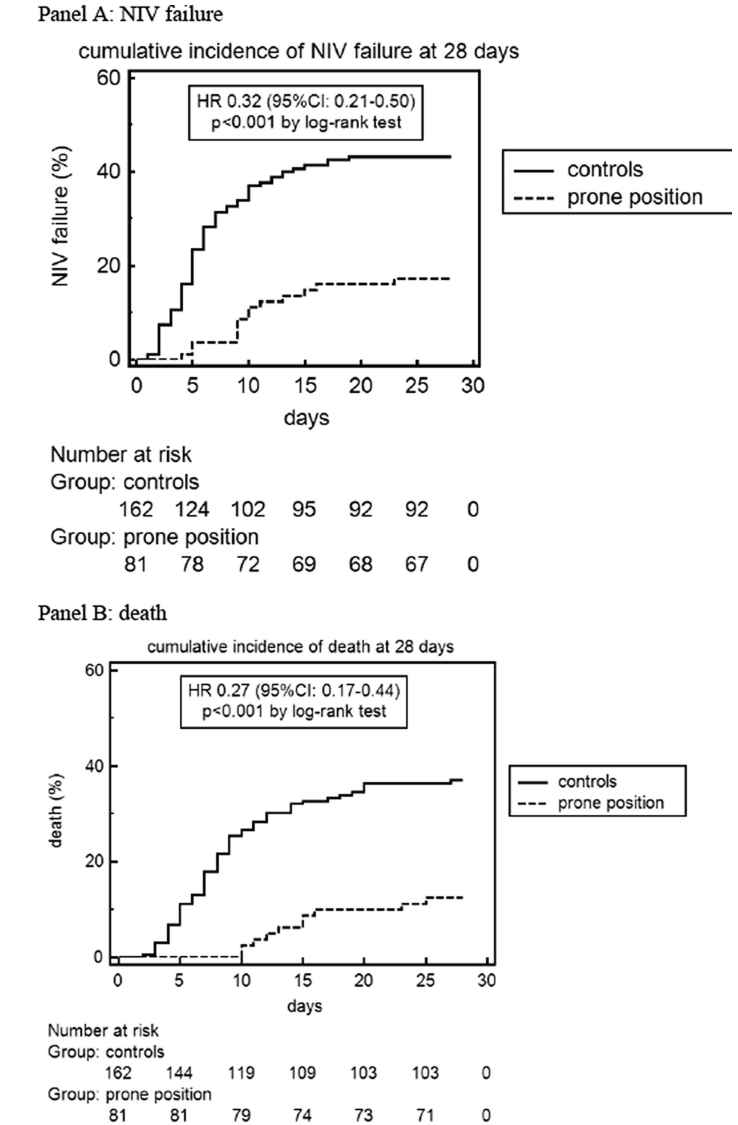
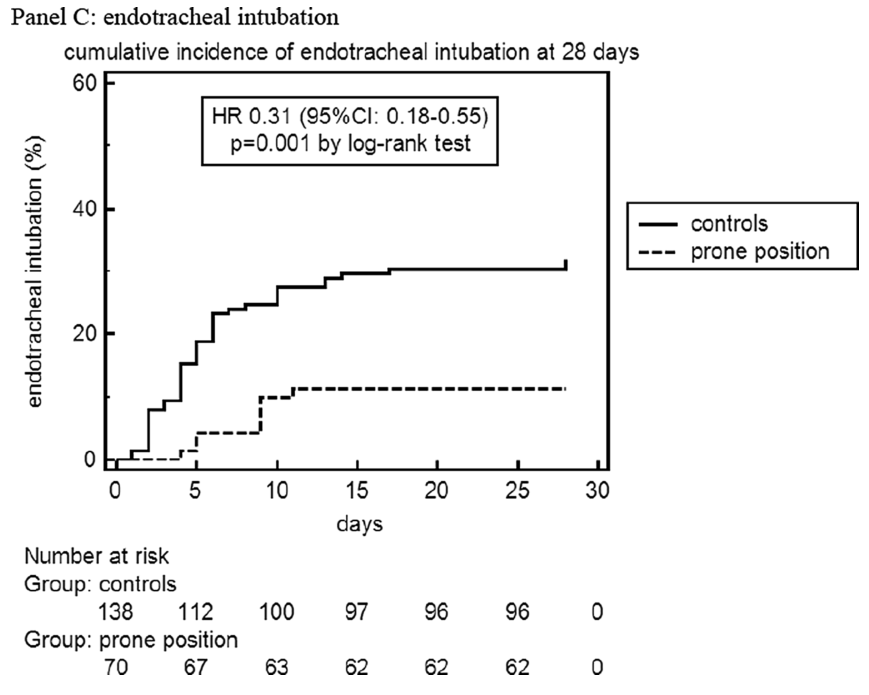
图1在入选后28天,俯卧位和对照组无创呼吸机(NIV)失败(A)、死亡(B)和气管插管(C)的累积发生率。在气管插管组中,排除了不插管(DNI)倾向的患者
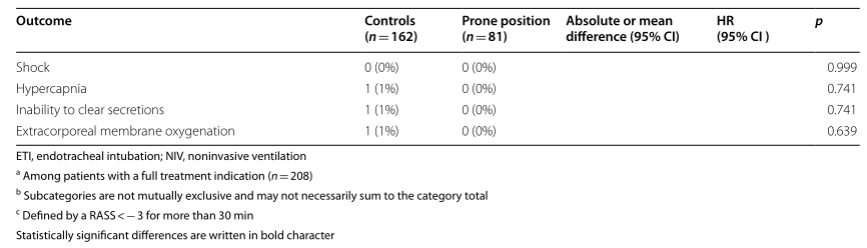
表1纳入初步(意向治疗)分析的患者在28天内的疗效和安全性结果,按研究干预措施分组(n=243)
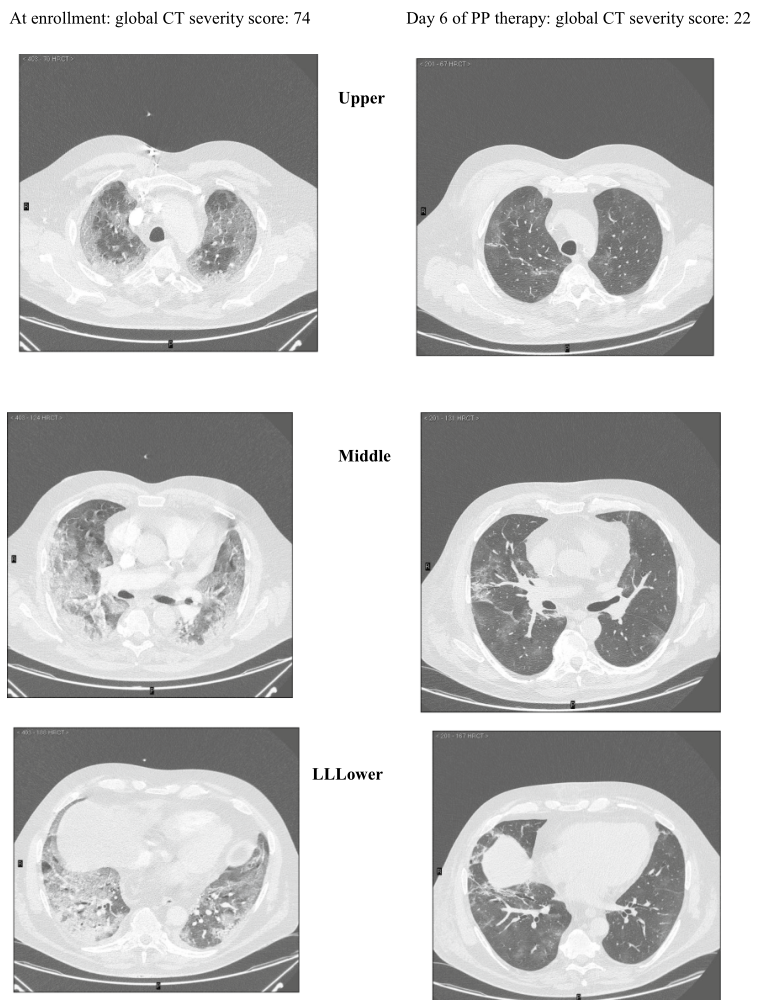
患者A:55岁男性,入院时PaO2/FiO2=75毫米汞柱
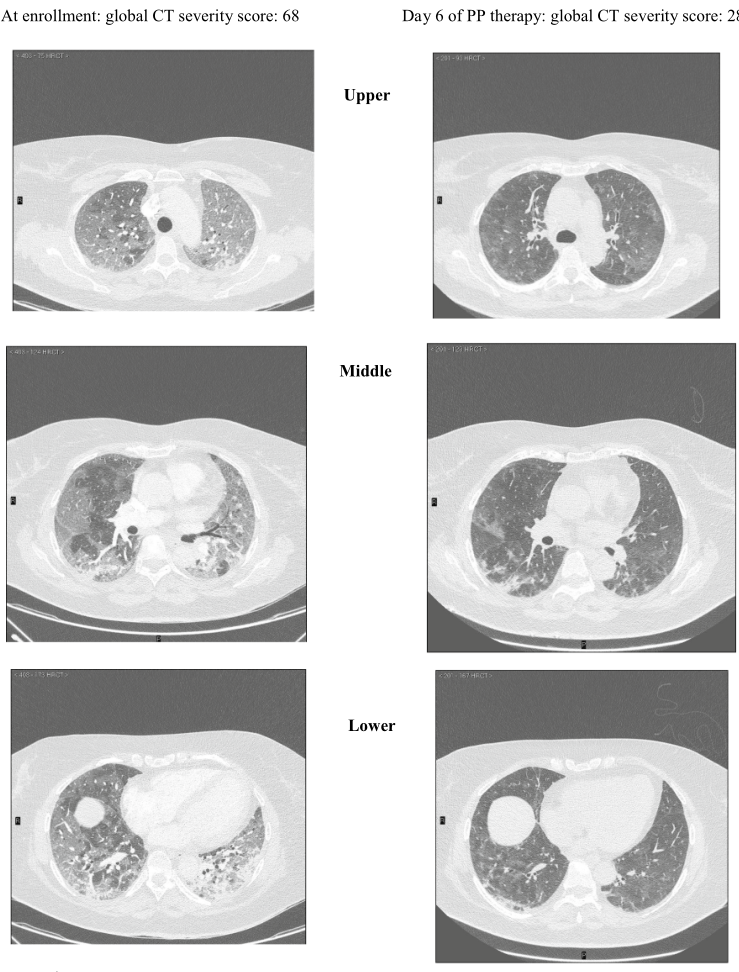
患者B:一位60岁的肥胖女性(登记时PaO2/FiO2=72毫米汞柱)
图2 根据Salaffi等人验证的评分,对肺实质受累的程度和性质在三个水平(上、中、下)进行量化。(得分范围0-96)。下面提供了两例治疗前后的CT扫描
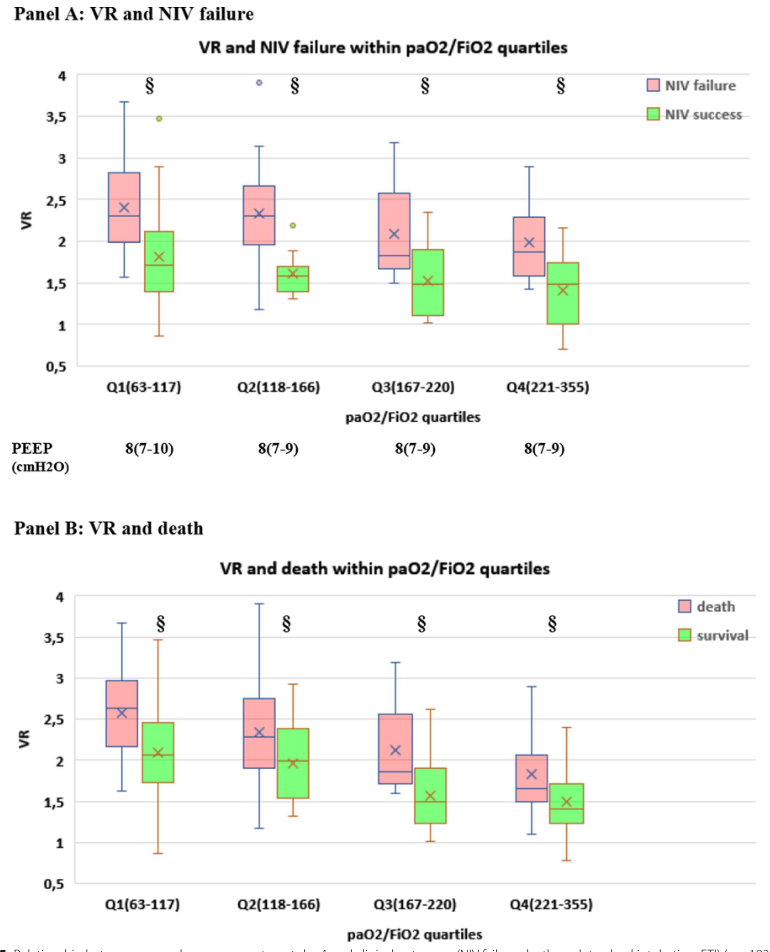
图5第1天气体交换参数与临床结果(NIV失败、死亡、气管插管、ETI)的关系(n=182)。死腔指数通气率(VR)与Sp1时间点PaO2/FiO2四分位内NIV衰竭、死亡和ETI的A-C关系(即第1天的仰卧位,在PP组对应于第一次8h通宵PP治疗后的恢复)。每个四分位数内的PaO2/FiO2范围和进行测量的PEEP(中位数,IQR)报告在面板的底部。§四分位数内治疗失败与P<0.001。氧气反应和二氧化碳反应对NIV失效、死亡和ETI的同时影响。通过通气率(VR)评估二氧化碳反应。与其他组相比p<0.001;与其他组相比p<0.001
结论:新冠肺炎相关性中重度低氧性呼吸衰竭患者早期延长PP是安全的,与较低的NIV失败率、插管率和病死率有关。在我们的研究人群中,早期死腔缩小和肺背侧区域的复氧可以预测临床结果。
原文出处:Musso G, Taliano C, Molinaro F,et al.Early prolonged prone position in noninvasively ventilated patients with SARS-CoV-2-related moderate-to-severe hypoxemic respiratory failure: clinical outcomes and mechanisms for treatment response in the PRO-NIV study.Crit Care 2022 Apr 29;26(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#无创呼吸机#
73
#SARS-CoV#
90
#临床结果#
72
#相关性#
72
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
80
#呼吸机#
77
#SARS#
95
#俯卧位#
70