Anesthesiology:年轻患者术后不得不吃的“灵丹”---ARBs
2015-08-22 MedSci MedSci原创
血管紧张素受体阻滞剂(ARBs)是高血压治疗药物的一种,同时具有延缓肾脏病进展以及逆转左室肥厚和血管重塑的作用。然而,尽管ARBs已经在临床上广泛使用,有关ARBs围术期管理的指南还并不成熟。加利福尼亚大学的研究人员针对接受ARBs治疗的退伍军人进行了一项队列研究,旨在探讨在术后早期停止ARBs的使用是否与术后发病率及死亡率相关。 在这项回顾性队列研究中,研究人员对1999-20
血管紧张素受体阻滞剂(ARBs)是高血压治疗药物的一种,同时具有延缓肾脏病进展以及逆转左室肥厚和血管重塑的作用。然而,尽管ARBs已经在临床上广泛使用,有关ARBs围术期管理的指南还并不成熟。加利福尼亚大学的研究人员针对接受ARBs治疗的退伍军人进行了一项队列研究,旨在探讨在术后早期停止ARBs的使用是否与术后发病率及死亡率相关。
在这项回顾性队列研究中,研究人员对1999-2011年间退伍军人医疗体系为退伍军人(非心脏手术)开具的ARBs常规处方,退伍军人术后ARBs使用的模式进行了评价。使用多变量和倾向分值匹配法考克思比例危险模式,检测术后2天没有继续使用ARB对全因30天死亡率的独立作用。
在本次研究招募的1,167,482例手术患者中,有30,173 位住院手术患者达到了入选标准。约有10,205位(33.8%)患者在术后第2天没有继续使用ARB。继续使用ARB的患者的30死亡率为1.3% (260/ 19,968),然而没有使用ARB的患者的30死亡率为3.2% (323 / 10,205) 。与继续使用ARB的患者相比,没有继续使用ARB的患者的30天死亡率未调整风险比(HR)为 2.45 (95% CI, 2.08 - 2.89; P < 0.001),然而多变量调整HR为1.74 (95% CI, 1.47 -2.06; P < 0.001)。当局限于一个只包含19,490位患者的倾向分值匹配的子集时,HR 是相似的 (1.47; 95% CI, 1.22 - 1.78; P < 0.001)。与老年患者相比(HR = 1.42; 95% CI, 1.09 - 1.85; 年龄 >75 yr P = 0.01),没有继续使用ARB的年轻患者死亡风险增加(HR = 2.52; 95% CI, 1.69 - 3.76; 年龄 <60 yr P < 0.001)。
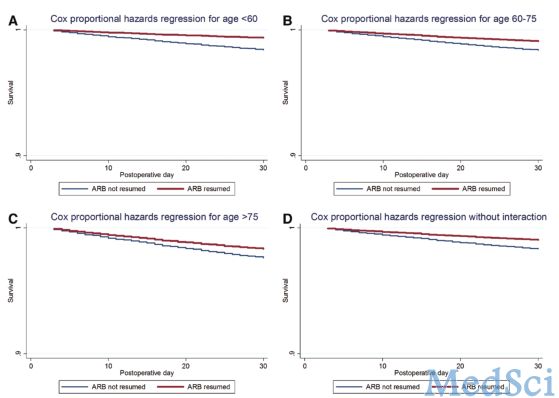
术后没有及时继续使用ARB的情况是很常见的,尤其是对于术后虚弱的患者。加利福尼亚大学的研究表明:术后没有继续使用ARB将导致患者(尤其是年轻患者)术后30天死亡率的风险大大增。
原始出处:
Susan M.Lee,F.R.C.P.C.,Steven Takemoto,Arthur W.Wallace. Association between Withholding Angiotensin Receptor Blockers in the Early Postoperative Period and 30-day Mortality Anesthesiology. 2015 Aug;123(2):288-306
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#EST#
61
#ARBs#
80
#年轻患者#
75
#ESI#
81