Clin Gastroenterology H:他克莫司和消炎痛可有效降低ERCP术后胰腺炎的发生率
2020-05-01 MedSci原创 MedSci原创
胆道并发症在肝移植患者中高达25%,并且通常通过内镜逆行胰胆管造影术(ERCP)进行处理。但是胰腺炎是ERCP之后最常见的不良事件。据报道他克莫司和消炎痛均可降低胰腺炎的风险。
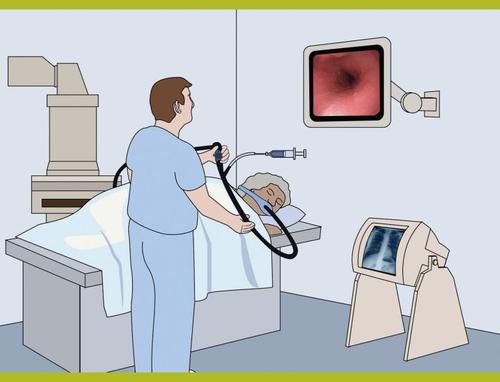
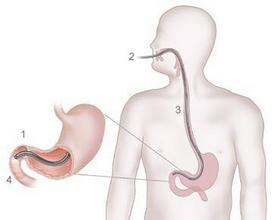
背景与目标: 胆道并发症在肝移植患者中高达25%,并且通常通过内镜逆行胰胆管造影术(ERCP)进行处理。但是胰腺炎是ERCP之后最常见的不良事件。据报道他克莫司和消炎痛均可降低胰腺炎的风险。本项研究旨在调查肝移植患者术后后接受ERCP后胰腺炎的发生率,以及他克莫司和/或消炎痛在降低胰腺炎风险方面的有效性。
方法: 研究人员从2007年6月1日至2015年12月1日对337例肝移植后胆道并发症进行ERCP(n = 937)的患者进行了回顾性研究。2012年6月1日之后,常规按100 mg剂量服用直肠消炎痛(100 mg),最终有286 例ERCP后给予消炎痛治疗。在排除急性/慢性排斥反应的患者之后,在ERCP之前,对323名患者进行了稳定剂量的他克莫司治疗(901例)。最后,研究人员收集了有关人口统计学和临床变量,术前他克莫司低谷水平以及PEP发生情况的数据。主要观察结果是胰腺炎的发生。次要结局包括发展为中度至重度胰腺炎,胆管炎和出血。
结果:ERCP程序后胰腺炎的发生率在2.2%左右。他克莫司的谷值高于2.5 ng/mL时,胰腺炎的机率降低了79%(OR,0.21; 95%CI,0.06-0.72;P = 0.01)。消炎痛可使胰腺炎风险降低91%(OR,0.09; 95%CI,0.01-0.85;P = .03)。消炎痛的使用不会影响出血或胆管炎的发生率或肾小球滤过率的降低。他克莫司谷浓度低于2.5 ng/mL的患者与不接受消炎痛的患者相比,消炎痛的添加可使胰腺炎的几率降低93%。(OR:0.07; 95%CI,0.01-0.90;P = .04)。
结论:本项研究发现他克莫司的谷水平超过2.5 ng/mL可以显着降低胰腺炎的风险。ERCP后直肠给予消炎痛治疗可显着降低胰腺炎的发生率,并进一步降低他克莫司的风险。两种药物的给药均可以防止患者发展为中度或重度胰腺炎。消炎痛不会使慢性肾脏病患者的肾功能恶化。
原始出处:
Nikhil R. Thiruvengadam. Et al. Tacrolimus and Indomethacin Are Safe and Effective at Reducing Pancreatitis After Endoscopic Retrograde Cholangiopancreatography in Patients Who Have Undergone Liver Transplantation. Clin Gastroenterology H.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
64
#发生率#
71
#GAS#
65
#Gastroenterol#
64
#他克莫司#
94
#Gastroenterology#
0