J Arthroplasty:TKA中髌骨去神经化带来的好处
2014-05-22 佚名 医学界骨科频道
全膝关节置换TKA可帮助膝关节炎患者迅速缓解疼痛恢复功能,但仍有20%的患者在术后因种种原因觉得疗效不满意。术后疼痛,尤其是膝关节前方疼痛给医生和患者带来不少烦恼。在手术中对髌骨进行假体置换的临床结果并不理想,与其相关的并发症如髌骨假体的磨损、髌骨骨折、髌腱断裂常常会增加后期返修手术的难度。【原文下载】 有多个浅表神经分布支配到髌骨,包括:大腿内侧皮神经、股骨后皮神经、膝关节内外侧支持带神经
全膝关节置换TKA可帮助膝关节炎患者迅速缓解疼痛恢复功能,但仍有20%的患者在术后因种种原因觉得疗效不满意。术后疼痛,尤其是膝关节前方疼痛给医生和患者带来不少烦恼。在手术中对髌骨进行假体置换的临床结果并不理想,与其相关的并发症如髌骨假体的磨损、髌骨骨折、髌腱断裂常常会增加后期返修手术的难度。【原文下载】
有多个浅表神经分布支配到髌骨,包括:大腿内侧皮神经、股骨后皮神经、膝关节内外侧支持带神经。许多医生在手术中常规对其进行去神经化处理,而也有的医生只对术中存在髌股关节面磨损的髌骨进行去神经化。
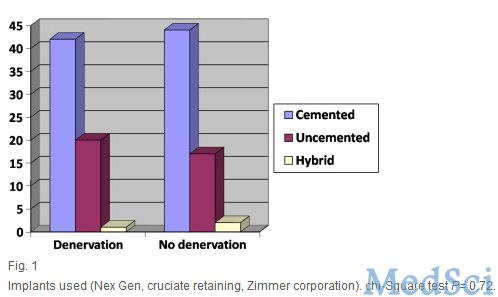
在2009年4月至2010年6月之间英国的Videsh V. Raut医生进行了一项髌骨去神经化的随机对照研究,发表在2014年5月的The Journal of arthroplasty杂志上。一组患者进行髌骨去神经化处理,另外一组患者不进行髌骨去神经化,每组63例患者。在术后3个月、12个月、24个月时对患者进行复查,评估膝关节各方面功能评分和活动度,去神经化组患者平均随访26.5个月,未去神经化组患者平均随访26.3个月。
在术后3个月时,去神经化处理的患者其膝关节前侧的疼痛情况要明显好于后者,但是在术后12个月和24个月时,两组患者的疼痛情况却相差不多。在各随访时间点,经过去神经化处理的患者其膝关节屈曲功能明显好于后者,但两组患者的剑桥膝关节评分、膝关节功能评分、髌骨评分等方面并无显著差异。
通过本次长达2年的随访研究,作者认为:全膝关节置换手术中对髌骨进行去神经化处理安全有效,虽然术后2年膝关节评分等功能评分方面和未进行去神经化处理的患者相似,但是通过去神经化处理的患者的满意度和膝关节屈曲活动度获得明显提高。
相关阅读:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AST#
62
#ART#
61
#髌骨#
76
#去神经化#
68
#TKA#
70