Cancer Cell:二甲双胍+轻断食,让癌细胞死亡!科学家发现二甲双胍联合低糖,可以显著抑制肿瘤生长
2019-05-14 奇点糕 奇点网
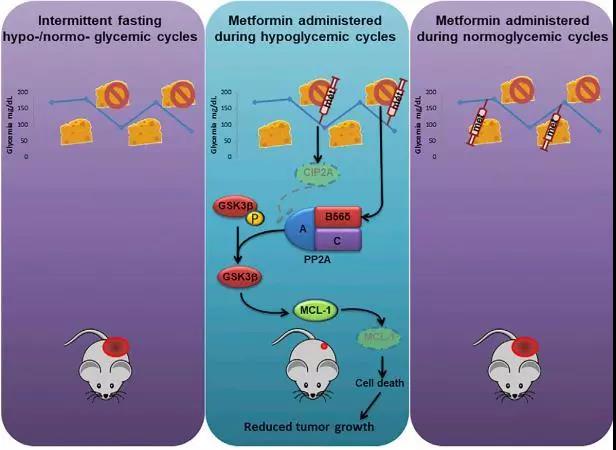
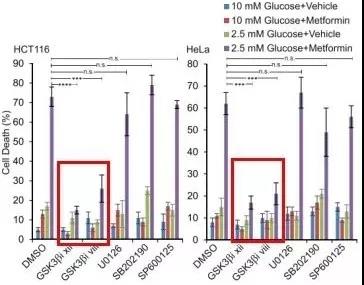
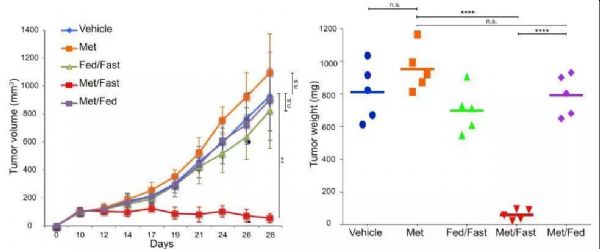
欧洲肿瘤研究所的学者们发现,二甲双胍和禁食可以协同作用,抑制小鼠肿瘤的生长。通过进一步研究发现,二甲双胍和禁食通过 PP2A-GSK3β-MCL-1通路抑制肿瘤生长。研究发表在Cancer Cell上。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抑制肿瘤#
96
#CEL#
65
#科学家发现#
75
#cancer cell#
80
#Cell#
65
#癌细胞#
61
#轻断食#
82
好
101
二甲双胍,神药!
77