Ann Surg:新辅助放疗VS.单纯手术治疗有或无高危因素的II/III期直肠癌的疗效
2021-05-09 MedSci原创 MedSci原创
新辅助放疗(NRT)通常用于II/III期直肠癌,以改善局部控制,同时不影响总体生存。然而,在某些患者中,仅靠高水平手术也可以达到良好的局部控制。近日,研究人员探究了有或没有高危因素的II/III期直
新辅助放疗(NRT)通常用于II/III期直肠癌,以改善局部控制,同时不影响总体生存。然而,在某些患者中,仅靠高水平手术也可以达到良好的局部控制。近日,研究人员探究了有或没有高危因素的II/III期直肠癌中新辅助放疗(NRT)的治疗效果,研究结果已发表于 Ann Surg。
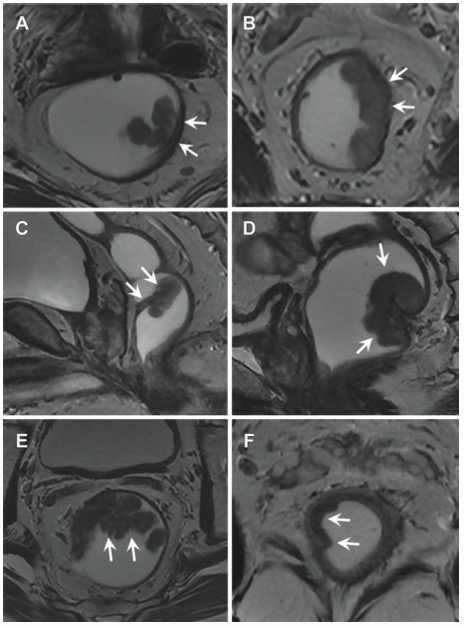
根据风险分层标准和临床分期,纳入符合条件的II/III期直肠癌参与者,术前分为有(高风险)或无(低风险)高风险因素的患者,分别随机接受短程放疗(SCRT)+全直肠系膜切除术(TME)或单纯TME,分为以下4组:高危患者接受(HiR)或不接受(HiS)放射治疗,低危患者接受(LoR)或不接受(LoS)放射治疗。主要终点是局部复发。次要终点包括总生存期、无病生存期、远处复发、手术质量和安全性。
共有401名患者纳入最终分析。中位随访54个月,低风险患者获得了比高风险患者更低的3年累计局部复发率(2.2% vs 11.0%,P = 0.006)和累计远处复发率(12.5% vs 29.4%,P < 0.001),更高的总生存率(86.9% vs 76.5%,P = 0.002)和无病生存率(87.0% vs 67.9%,P < 0.001)。关于局部复发的3年累积发生率,LoR组和LoS组(1.2% vs 3.0%,P = 0.983)或HiR组和HiS组(12.9% vs 8.9%,P = 0.483)之间没有差异。
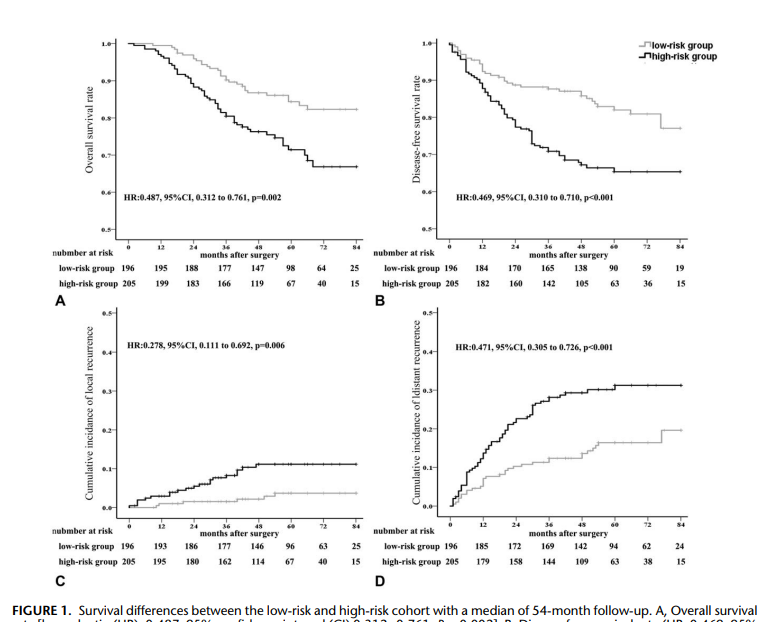
总之,该研究结果表明,根据风险因素对II/III期直肠癌进行分层,使之成为更精确的亚分类,可能会在存活率和局部复发控制方面产生差异。仅仅通过前期良好的手术质量,就可以在低风险患者中实现极低的局部复发累积发生率和生存率。研究的局限性在于不能证明单纯手术的非劣效性,建议根据II/III期直肠癌的临床风险分层,有针对性地使用NRT。
原始出处:
Xiangbing Deng, et al., Neoadjuvant Radiotherapy Versus Surgery Alone for Stage II/III Mid-low Rectal Cancer With or Without High-risk Factors: A Prospective Multicenter Stratified Randomized Trial. Ann Surg. 2020 Dec;272(6):1060-1069. doi: 10.1097/SLA.0000000000003649.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新辅助#
70
#新辅助放疗#
76
#III#
74
#手术治疗#
72
#辅助放疗#
101
#III期#
90
谢谢梅斯提供这么好的信息,学到很多
85