IBD: 肠道超声评估肠道行为可以预测克罗恩病患者对抗TNF治疗的早期反应
2022-01-13 MedSci原创 MedSci原创
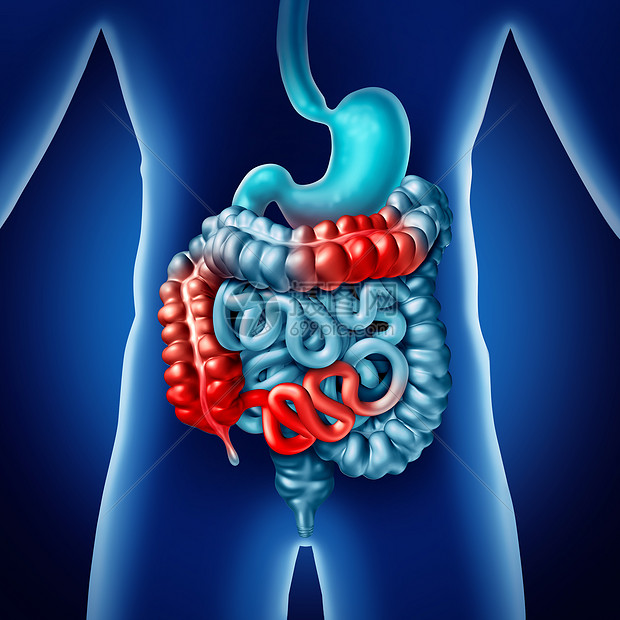
克罗恩病是一种消化道的慢性、反复发作和非特异性的透壁性炎症, 病变呈节段性分布, 可累及消化道任何部位,其中以末端回肠最为常见,结肠和肛门病变也较多。
抗肿瘤坏死因子(TNF)-α药物(如英夫利昔单抗)被广泛用于治疗CD患者,特别适用于频繁复发、严重疾病活动期和预后不良的患者。然而,高达40%的患者对抗TNF-α药物没有反应,大约10%的患者有药物不良反应,从而影响治疗。因此,在 "严格控制 "和 "对症下药 "策略的时代,预测和监测抗TNF-α治疗的反应至关重要。有一些研究结果表明C反应蛋白、粪钙卫蛋白、黏膜变化和横断面成像评估的透壁损伤与接受抗肿瘤药物的CD患者的治疗结果有关。内镜检查是评估CD患者在接受抗肿瘤药物治疗3-6个月内疗效的金标准。鉴于在短期随访中频繁进行内窥镜评估因其侵入性而无法实施,因此,临床上需要另一种客观的、容易重复的、但无创的评估方法。
作为CD的一种横断面成像方式,肠道超声已被推荐使用,并已被广泛用于评估CD肠道的变化。以前的研究已经证明,剪切波弹性成像(SWE)是一种可行的、准确的超声弹性成像方式,可对CD患者的肠道纤维化进行无创性量化分析。据报道,纤维化的程度会影响抗肿瘤药物的治疗效果。因此,SWE可能有助于预测抗TNF治疗的早期反应,并可能成为肠道纤维化改善的一个指标。因此,本项研究旨在探究 (a) 通过超声接受抗 TNF 治疗的 CD 患者肠道行为发生的变化;(b) 剪切波弹性成像 (SWE) 在预测对抗 TNF 治疗的早期反应方面的可行性。
研究人员将存在回肠或回结肠CD并接受抗TNF治疗的患者纳入本项研究。研究人员对所有患者在基线和第 2、6 和 14 周进行肠道超声检查。使用线性混合模型比较肠壁厚度、肠壁多普勒信号(Limberg 评分)和 SWE 值的变化。主要观察指标是抗 TNF 治疗的早期反应以及基于第 14 周临床和结肠镜检查结果。

本研究纳入的 30 例患者中,有 20 例患者在第 14 周对抗 TNF 治疗产生反应。与无反应组相比,反应组的肠壁厚度和 SWE 值呈显着下降趋势(P =0.003)。与基线相比,响应组的肠壁厚度、Limberg 评分和 SWE 值早在第 2 周就显着降低(P <0.001)。无反应组的基线 SWE 值(21.3±8.7 vs. 15.3±4.7 kPa,P=0.022)和肠壁厚度(8.5±2.3 vs. 6.9±1.5 mm,P = 0.027)显着高于有反应组患者。
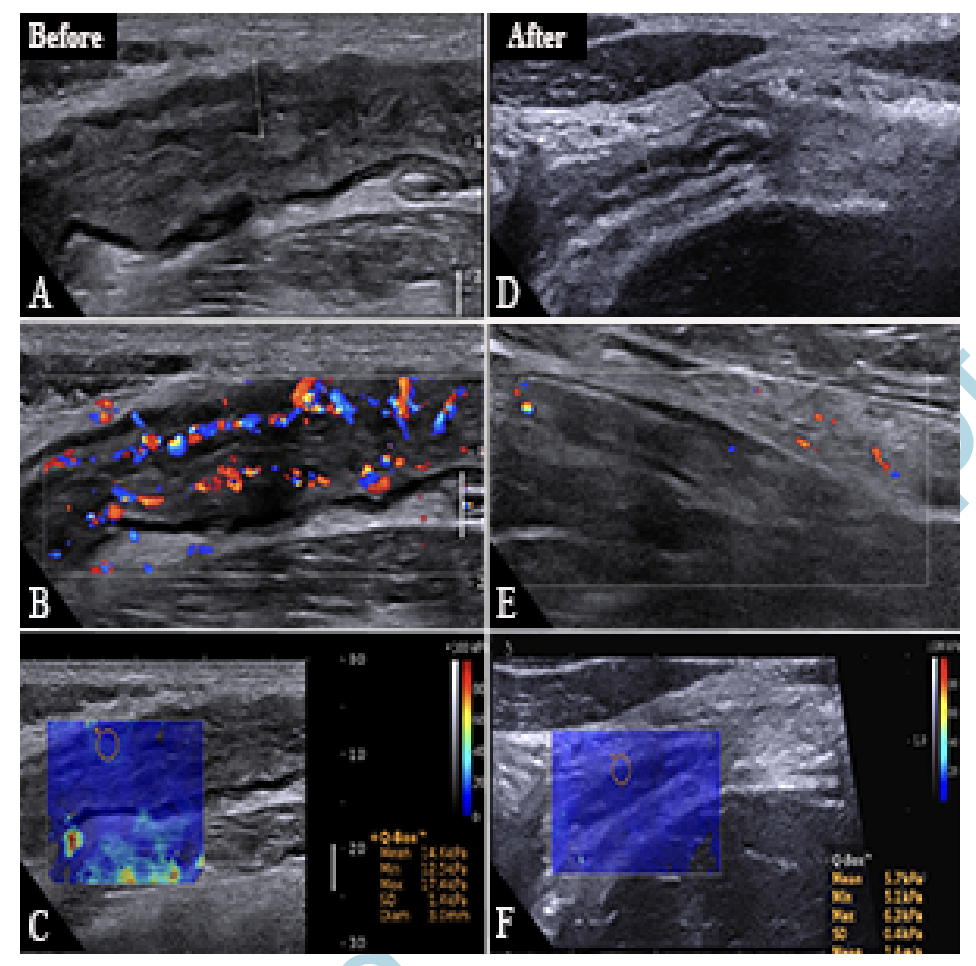
图:B超展示肠道病变情况
本项研究最后证实最早可以在开始抗 TNF 治疗后的第 2 周评估肠道超声行为的变化,可以通过肠道超声和弹性成像来预测抗 TNF 治疗的早期反应。
原始出处:
Yu-Jun Chen. Et al. Longitudinal Bowel Behavior Assessed by Bowel Ultrasound to Predict Early Response to Anti-TNF Therapy in Patients with Crohn's Disease: A Pilot Study. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抗TNF#
58
#抗TNF治疗#
62
#超声评估#
57
#IBD#
49
#TNF#
60