Circulation:影响外周动脉疾病患者发生急性肢体缺血的风险因素
2019-08-18 MedSci MedSci原创
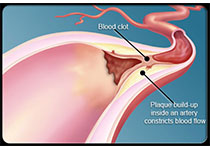
急性肢体缺血(ALI)是一个重要的临床事件,也是心血管临床试验一种新兴的预后结果。现研究人员对ALI后的风险因素和预后进行评估。将外周动脉疾病患者随机分至替格瑞洛组和氯吡格雷组。受试患者的纳入标准包括踝肱指数≤0.80或既往进行过下肢血管重建。根据主要预后、随机化分组后的住院情况将患者分层。共13 885位患者,其中232位(1.7%)患者共293次因ALI住院(0.8/100人·年)。有ALI的
将外周动脉疾病患者随机分至替格瑞洛组和氯吡格雷组。受试患者的纳入标准包括踝肱指数≤0.80或既往进行过下肢血管重建。根据主要预后、随机化分组后的住院情况将患者分层。
共13 885位患者,其中232位(1.7%)患者共293次因ALI住院(0.8/100人·年)。有ALI的患者和无ALI的患者相比,年龄更小,且更常有周围血管重建和较低的踝肱指数基线。ALI住院期间的治疗包括血管内血运重建(39.2%,115例)、旁路搭桥(24.6%,72例)和大截肢(13.0%,38例)。经多变量校正后,任何既往外周血管重建、房颤和起始踝肱指数≤0.60都与ALI风险更高相关(危险比[HR]分别是4.7、1.8和1.3/降低0.1,p<0.01)。年长与应用他汀类药物均与ALI风险更低相关。替格瑞洛和氯吡格雷治疗对ALI风险的影响无差别。对于既往进行过血管重建的患者,与血管内血运重建相比,6个月以前进行过旁路搭桥可增加ALI风险(HR 2.63)。在总人群中,ALI住院会增加随后MACE、全因死亡和大截肢的风险(HR分别是1.4、3.3和34.2)。
原始出处:
Connie N. Hess ,et al.Acute Limb Ischemia in Peripheral Artery Disease. Circulation. 2019;140:556–565. https://doi.org/10.1161/CIRCULATIONAHA.119.039773
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疾病患者#
73
#外周动脉#
58
学习了,学习了
66
学习了很有用不错
74
学习了
74
好好好好好好
84
学习了,谢谢分享
77
好
50