Brit J Sports Med:澳Meta分析称,治疗外周动脉疾病,练肌肉可明显缓解症状
2019-08-11 朱柳媛 中国循环杂志
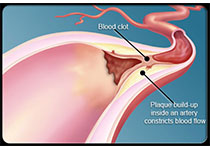
目前的外周动脉疾病治疗指南建议,一旦确诊下肢动脉疾病,运动是首要的初始治疗措施,间歇走路是改善症状的金标准。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#练肌肉#
73
#Meta#
41
#MET#
52
#外周动脉#
0
#Med#
53
学习了,谢谢分享。
84