JCO:这种癌也被过度诊断了?CSCO专家呼吁为其改名!
2022-04-26 MedSci原创 MedSci原创
专家认为取消GS6的癌症标签将极大地改善个人和公共健康。而这类患者需要做的只是采取积极监测,而无需立即采取治疗。
前列腺特异性抗原(PSA)是检测前列腺癌的重要指标,然而PSA筛查对前列腺癌(PCa)仍有很大争议,主要是因为不清楚降低转移率和癌症死亡率的主要好处是否值得过度诊断、过度治疗和潜在的治疗相关疾病的风险。
导致过度诊断和过度治疗的一个主要因素是将前列腺中特定的低级细胞变化模式定为癌症。近期,来自CSCO的专家在《临床肿瘤学杂志》(Journal of Clinical Oncology)发文指出,低级别前列腺癌不应该再被称为癌症。对这些病变进行简单的术语修改,并去掉癌症的标签,将大大减少过度诊断和过度治疗,并明显改变PSA筛查的成本-效益计算。
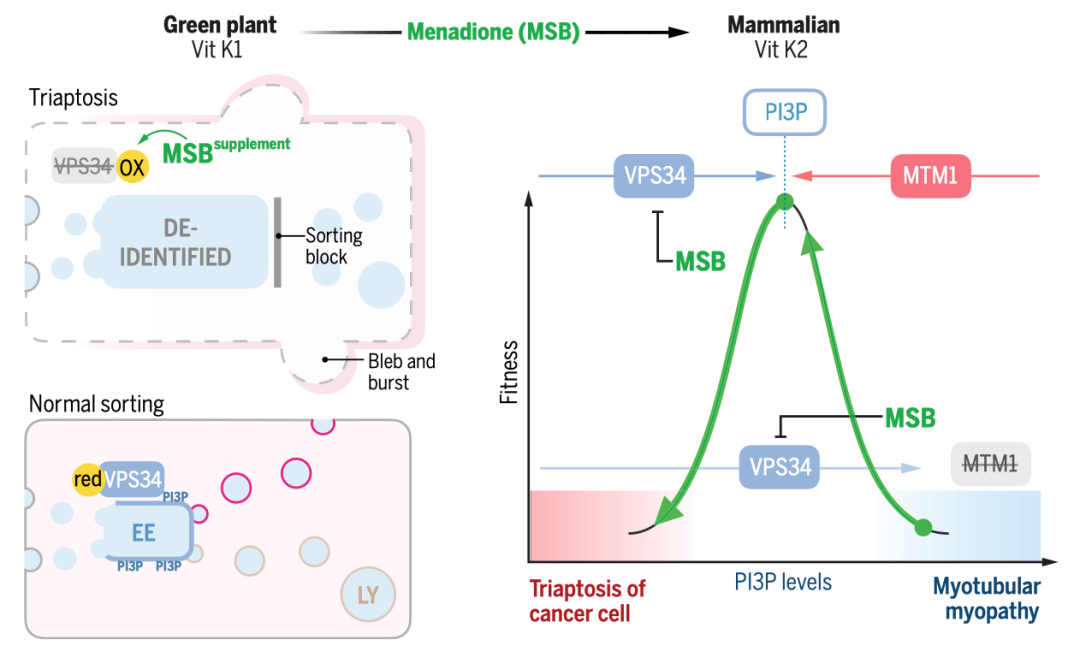
过度诊断流行病的根源在于50岁以上的男性中>30%(到80岁时>60%)会出现组织学PCa,因为如果一个人活得足够长,几乎所有的前列腺都会最终发展出微小的PCa。病理学结果GS6(即Gleason评分为6,为低级别)是一种自然的、与年龄有关的组织学观察,被人为地定义为一种疾病,不知道会引起症状或转移,但矛盾的是导致侵入性监测或治疗。这些担忧是导致美国预防服务工作组在2012年明确不鼓励PCa筛查的一个主要因素,特别指出了对 "微小的、分化良好的病变......不太可能有临床意义 "的常见诊断和治疗。
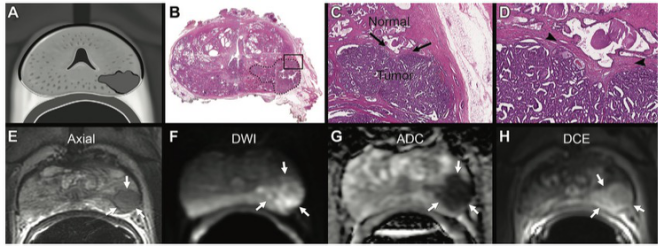
虽然GS6符合癌症的病理标准(侵入基质),但如果没有同时存在更高等级的疾病(GS≥7;即等级组≥2),它实际上不可能侵入邻近的局部结构或发生转移。当手术切除前列腺并术后证实为GS6时,尽管癌症通常已存在多年,甚至几十年,基本上100%不会发生转移。当癌症相关的死亡率接近0%,甚至在没有治疗的情况下也是如此,是时候应考虑修改筛查、诊断、管理和术语模式。
此外,无论医生花多少时间来淡化GS6诊断的重要性或强调低风险,"你得了癌症 "这句话对大多数男性和他们的家人都有强大的心理影响。
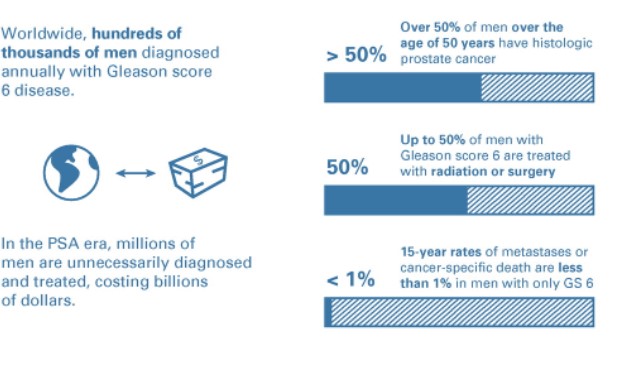
GS6患者15年内转移/死亡率低于1%
尽管与癌症相关的风险可以忽略不计,但PCa的诊断与抑郁症和自杀的风险增加有关,即使是低级别的PCa。同时,过度治疗往往会带来性功能障碍或尿失禁等副作用。而既往研究结果显示,低级别前列腺癌患者15年内转移/死亡率甚至低于1%。
因此,专家认为取消GS6的癌症标签将极大地改善个人和公共健康。而这类患者需要做的只是采取积极监测,而无需立即采取治疗。
参考文献:
Low-Grade Prostate Cancer: Time to Stop Calling It Cancer. Low-Grade Prostate Cancer: Time to Stop Calling It Cancer. https://ascopubs.org/doi/full/10.1200/JCO.22.00123
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCO#
100
同感
100
#专家呼吁#
118
甲状腺癌是否也存在类似情况?
115
学习
122