Allergy Asthma Proc:奥洛他定-莫米松组合鼻喷剂在季节过敏性鼻炎患者中的效果和安全性评估
2019-05-19 AlexYang MedSci原创
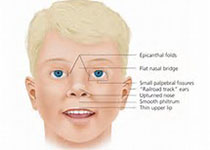
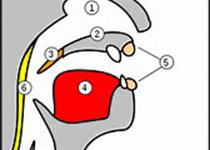
GSP301是一种研究用的固定剂量组合鼻喷剂,其中包含了抗组胺剂、盐酸洛普他定(HCI)和皮质类固醇糠酸莫米他松。最近,有研究人员评估了GSP301在季节过敏性鼻炎(SAR)患者中的效果和安全性。研究是一个双盲、随机和平行的研究。研究总共包括了1180名患者。在经过14天的治疗后,与安慰剂组(最小平方平均差-0.98;95%CI,-1.38到-0.57;p<0.001)和奥洛他定治疗组(p=
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ROC#
92
#莫米松#
73
#AST#
101
#asthma#
119
#过敏性#
67
#ALL#
46
#季节#
107
#PRO#
75
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
78