Eur Urol Focus:无夹机器人辅助根治性前列腺切除术及对结果的影响
2021-07-24 AlexYang MedSci原创
在进行机器人辅助前列腺根治术(RARP)时,使用手术夹对侧前列腺蒂进行无热解剖,并在盆腔淋巴结清扫术(PLND)期间进行结扎已成为手术过程的金标准。夹子的使用是为了防止无髓神经纤维和淋巴结的热损伤。
在进行机器人辅助前列腺根治术(RARP)时,使用手术夹对侧前列腺蒂进行无热解剖,并在盆腔淋巴结清扫术(PLND)期间进行结扎已成为手术过程的金标准。夹子的使用是为了防止无髓神经纤维和淋巴结的热损伤。

近期,有研究人员比较了一种新的无夹、侧蒂控制和PLND的双极能量RARP(RARP-bi)技术与标准的带夹RARP技术(RARP-c)的肿瘤学和功能结果。

研究人员在2018年7月至2020年3月期间对接受RARP的338名男性进行了一项回顾性研究。手术包括RARP-c与RARP-bi。他们前瞻性地收集了数据,并回顾性地比较了人口统计学、临床病理学和功能结果数据。使用扩展的前列腺癌临床实践指数评估了排尿以及性功能,并使用Clavien-Dindo分级评估了并发症。多变量回归模型调查了RARP-bi与RARP-c技术是否与手术边缘阳性(PSMs)或性功能和泌尿功能评分有关。
共有144名(43%)和194名(57%)男性分别接受了RARP-bi和RARP-c手术。总的来说,这两种方法在功能和肿瘤学结果上没有差异。在多变量回归分析中,RARP-bi技术与PSMs(OR=1.04,95%CI 0.6-1.8;P=0.9)、性功能(OR=0.4,95%CI 0.1-1.5;P=0.8)或泌尿功能(OR=0.5,95%CI 0.2-1.4;P=0.2)方面的显著差异没有关系。两组的30天总并发症率(12% vs 16%,p=0.5)和膀胱颈挛缩率(2.1% vs 3.6%,p=0.5)相似。另外,两组之间的淋巴囊肿并发症没有差异(1.4% vs 0.52%,p=0.58)。所有并发症均为Clavien-Dindo I-II级。
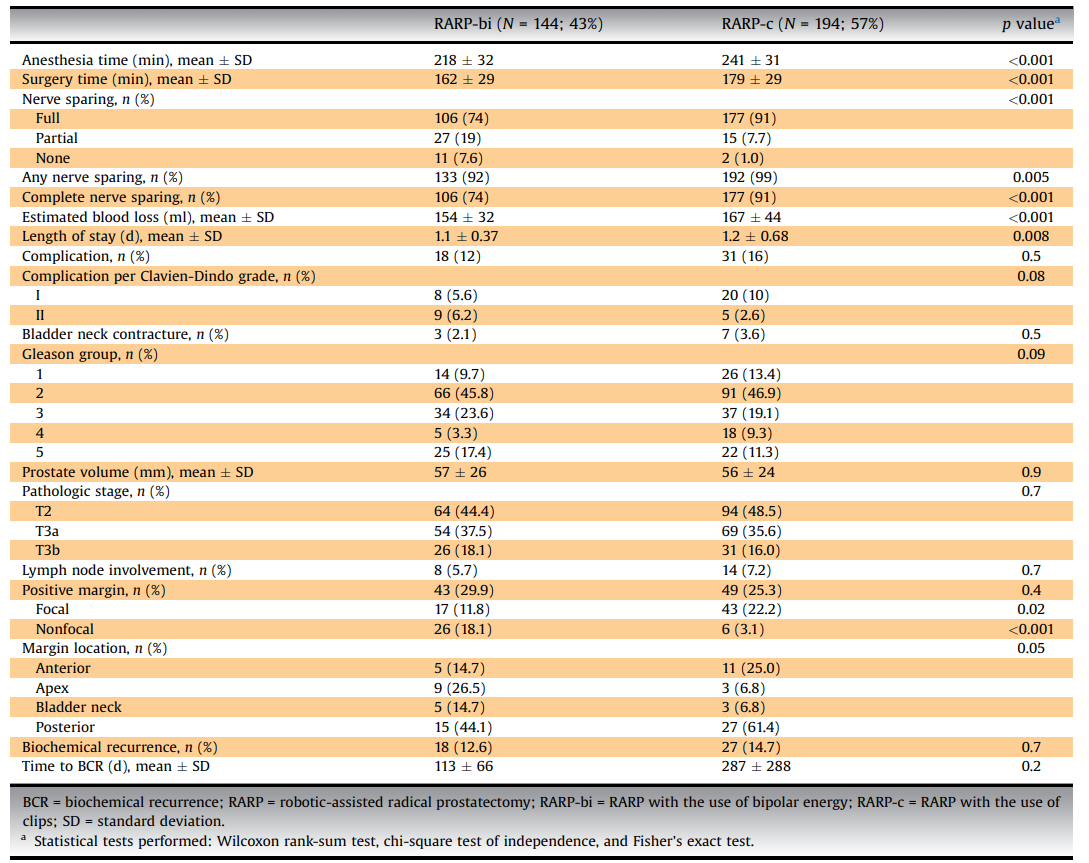
围手术期和手术后的结果
综上所述,尽管有人担心使用双极能量进行前列腺蒂剥离会增加神经损伤的风险,但研究结果证明该种技术在肿瘤学和功能上的结果与使用手术夹的标准方法相似,有夹和无夹技术在并发症或淋巴结形成方面也没有区别。
原始出处:
Spyridon P Basourakos , Patrick J Lewicki , Ashwin Ramaswamy et al. Clipless Robotic-assisted Radical Prostatectomy and Impact on Outcomes. Eur Urol Focus. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
59
#前列腺切除#
64
#机器人#
60
#机器人辅助#
120
#机器#
63
#根治#
121
非常受用
79
学习#学习#
123
学到了
81