Ann Oncol:纳武利尤单抗(Nivolumab)联合卡铂、紫杉醇和贝伐珠单抗一线治疗 晚期非鳞状非小细胞肺癌的疗效和安全性
2021-06-26 yd2015 MedSci原创
纳武利尤单抗(Nivolumab)联合卡铂、紫杉醇和贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌是一种可行的新策略。
非小细胞肺癌(NSCLC)是肺癌常见一种类型,约占85%。驱动基因阴性的晚期NSCLC标准一线治疗为免疫联合化疗。但是大部分联合化疗不包括抗血管治疗,比如常用的贝伐珠单抗。ONO-4538-52/TASUKI-52 (NCT03117049)是一项国际、多中心、随机、双盲、安慰剂对照的III期临床研究,评估纳武利尤单抗(Nivolumab)联合卡铂、紫杉醇和贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌的疗效和安全性。相关成果发表在Annals of Oncology杂志上。

该研究是在韩国、日本和我国台湾进行的,纳入2017年6月至2019年7月期间,既往未治疗的IIIB/IV期或复发性非鳞状NSCLC患者,这些患者没有EGFR、ALK或ROS1等基因突变。随机分配至纳武利尤单抗(Nivolumab)或安慰剂联合卡铂、紫杉醇和贝伐珠单抗治疗,每3周1疗程,最多6周期,之后纳武利尤单抗或安慰剂联合贝伐珠单抗维持治疗至疾病进展或不可耐受毒性反应。主要终点为由独立放射学审查委员会(IRRC)评估的无进展生存期(PFS)。
共纳入550例患者,分别有273例和275例患者接受了nivolumab和安慰剂组治疗。中位年龄为66岁,两组有吸烟史患者分别有77.8%和80.4%。两组PD-L1阴性的比例均为43.6%。
两组的中位PFS分别为12.1个月 (96.37% CI, 9.8–14.0) 和8.1个月 (96.37% CI, 7.0–8.5)。nivoluma组较安慰剂组降低了44%的无进展风险(HR=0.56; 96.37% CI, 0.43–0.71; P < 0.0001) 。两组的12个月PFS率分别为50.1%和30.2%。大部分亚组均可从nivolumab获益。
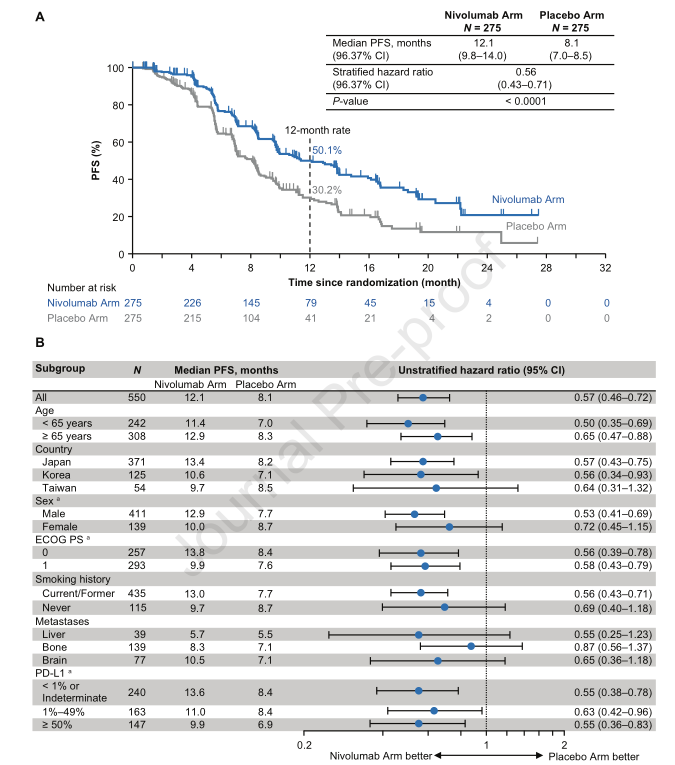
总人群两组治疗和亚组分析PFS
对PD-L1分层分析时,无论PD-L1表达水平,nivolumab组较安慰剂组均取得PFS获益。PD-L1阴性时,nivolumab组和安慰剂组的中位PFS分别为13.6个月和8.4个月(HR=0.55 (95% CI, 0.38–0.78),p < 0.0001);PD-L1 1%–49%时,nivolumab组和安慰剂组的中位PFS分别为11个月和8.4个月(HR= 0.63 (95% CI, 0.42–0.96));PD-L1≥50%时,nivolumab组和安慰剂组的中位PFS分别为9.9个月和6.9个月(HR= 0.63 (95% CI, 0.42–0.96))。

PD-L1分层分析两组PFS
两组的中位OS分别为25.4个月和24.7个月,两组没有统计学差异(HR= 0.85 (95% CI, 0.63–1.14),p= 0.2754)。
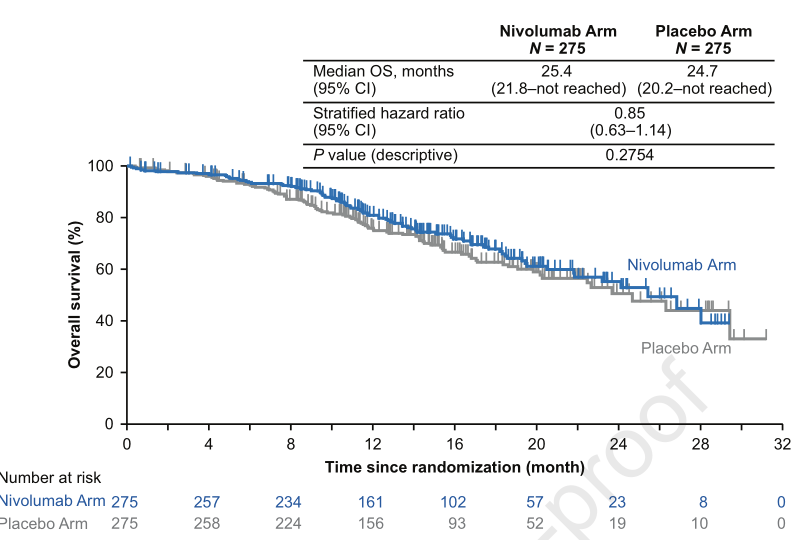
两组的OS
IRRC评估的ORR分别为61.5%和50.5%(OR=1.55 (95% CI, 1.11–2.17));中位缓解持续时间分别为11.0个月和7.0个月。
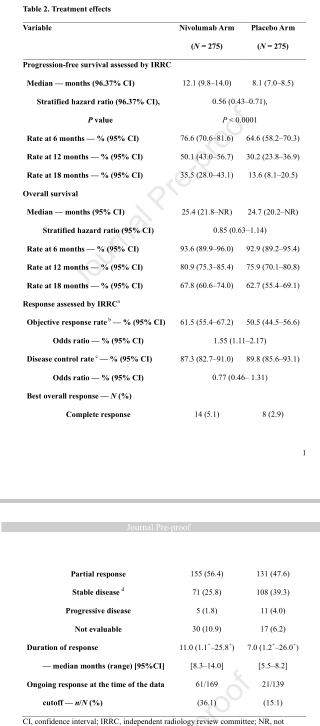
疗效评估
两组任何级别治疗相关不良事件(AEs)分别为98.5% (269/273) 和99.6% (274/275);两组常见3/4级AEs为中性粒细胞减少,发热性中性粒细胞减少,白细胞计数下降和高血压。两组周围神经病变分别为65.6%和65.5%。皮疹是两组最常见的免疫介导的不良事件,分别为41.0% 和17.1%。两组贝伐珠单抗相关的不良事件常见为高血压(23.8%和28.7%)、蛋白尿(23.8%25.1%),鼻出血(15.8%和13.8%)。
综上,研究表明,纳武利尤单抗(Nivolumab)联合卡铂、紫杉醇和贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌是一种可行的新策略。
原始出处:
S Sugawara, J-S Lee, J-H Kang, et al. Nivolumab with carboplatin, paclitaxel, and bevacizumab for first-line treatment of advanced non-squamous non-small cell lung cancer. Ann Oncol. 2021 Jun 14;S0923-7534(21)02052-4. doi: 10.1016/j.annonc.2021.06.004. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非小细胞#
88
#铂#
79
#mAb#
93
#NIV#
89
#贝伐珠#
72
研究表明,纳武利尤单抗(Nivolumab)联合卡铂、紫杉醇和贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌是一种可行的新策略。
111
#疗效和安全性#
76
#Oncol#
77
学习
121
#卡铂#
89