Lancet:不打针不吃药治疗高血压
2017-12-03 杨中华 脑血管病及重症文献导读
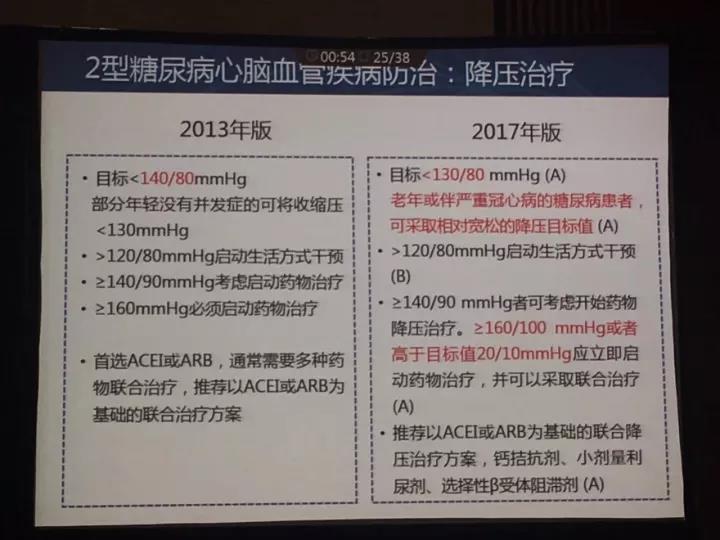
Esler等发现肾脏去神经支配以降低肾脏和全身交感张力,早期临床试验也发现这是一种有希望的方法。但是SYMPLICITY HTN-3试验并未发现肾脏去神经支配能够显著降低患者的血压(vs 假治疗,sham treatment)。事后分析推测以下因素是该研究未成功的原因:内科治疗依从性、肾脏去神经支配治疗不完全以及纳入了单纯收缩期高血压患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
50
lancet
85
学习.谢谢分享
74
很好的文章.谢谢分享!
102