Arthritis Rheumatol:英夫利昔单抗vs.阿达木单抗治疗难治性白塞病葡萄膜炎的比较研究
2019-06-27 xiangting MedSci原创
尽管IFX和ADA均对难治性BD葡萄膜炎有疗效,但在1年随访后,使用ADA治疗的结局比IFX更好。
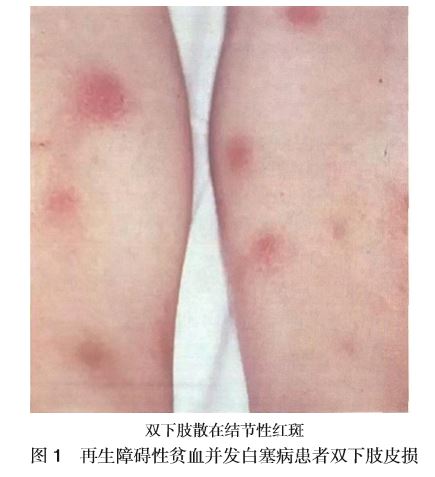
这项研究目的是在一个大型难治性白塞病(BD)葡萄膜炎患者队列中,比较1年期间英夫利昔单抗(IFX)与阿达木单抗(ADA)作为首个生物性药物的疗效。
这是一项开放标签多中心研究,使用IFX或ADA治疗常规非生物治疗无效的BD-葡萄膜炎患者。经过医生和患者同意后,选择IFX或ADA作为首个生物性治疗。给药方案为:IFX:第0、2、6周和此后每4-8周静脉注射3-5mg/kg,ADA:每两周40mg/s.c,无负荷剂量。对IFX和ADA治疗的患者进行比较。
纳入177例患者(316只眼睛受累)。103例患者使用IFX和74例使用ADA。基线时IFX组与ADA组间的主要人口学特征、既往治疗和眼部严重程度没有显著差异。治疗1年后,观察到两组的眼部指标均有所改善。然而,ADA疗法在某些指标上的结果更好,即在某些情况下有统计学显著差异:前房炎症(IFX组78.18%vs ADA组92.31%; p=0.06)、玻璃体炎(78.95%vs 93.33%;p=0.04)、视网膜血管炎(97%vs 95%;p=0.28)、黄斑厚度(264.89±59.74 vs 250.62±36.85;p=0.15)、最佳矫正视力(0.67±0.34 vs 0.81±0.26;p=0.001)和药物保留率(84.95%vs 95.24%;p=0.042)。
尽管IFX和ADA均对难治性BD葡萄膜炎有疗效,但在1年随访后,使用ADA治疗的结局比IFX更好。
原始出处:
Belén Atienza‐Mateo. Comparative study of infliximab versus adalimumab in refractory uveitis due to Behcet's disease, National multicenter study of 177 cases. Arthritis Rheumatol. 25 June 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Arthritis#
62
#ART#
71
#难治性#
58
#阿达木#
70