NEJM:派姆单抗治疗持续性、复发性或转移性宫颈癌的效果如何?
2021-11-11 MedSci原创 MedSci原创
在同时接受联合或不联合贝伐珠单抗化疗的持续性、复发性或转移性宫颈癌患者中,派姆单抗组的无进展生存期和总生存期显著长于安慰剂组。
派姆单抗对化疗期间进展的程序性死亡配体1(PD-L1)阳性转移性或不可切除的宫颈癌有效。

近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员旨在评估伴有或不伴有贝伐单抗的化疗方案中加入派姆单抗的相对益处。
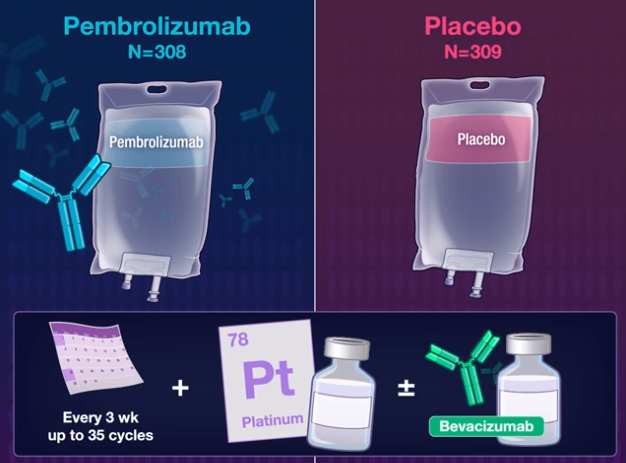
在这项双盲3期试验中,研究人员以1:1的比例随机分配患有持续性、复发性或转移性宫颈癌的患者,每3周接受派姆单抗(200mg)或安慰剂治疗,最多35个周期铂类药物化疗。该研究的双重主要终点为无进展生存期和总生存期,分别在PD-L1综合阳性评分为1或更高的患者、意向治疗人群和PD-L1综合评估10分或以上的患者中依次进行。综合阳性评分定义为PD-L1染色细胞数除以存活肿瘤细胞总数,再乘以100。所有结果均来自方案指定的第一次中期分析。
在548名PD-L1综合阳性评分为1或更高的患者中,派姆单抗组的中位无进展生存期为10.4个月,安慰剂组为8.2个月(疾病进展或死亡的风险比为0.62;95%置信区间[CI]为0.50至0.77;P<0.001)。在意向治疗人群的617名患者中,无进展生存期分别为10.4个月和8.2个月(风险比为0.65;95%CI为0.53至0.79;P<0.001)。在317名PD-L1综合阳性评分为10或更高的患者中,无进展生存期分别为10.4个月和8.1个月(风险比为0.58;95%CI为0.44至0.77;P<0.001)。派姆单抗组24个月时的总生存率为53.0%,安慰剂组为41.7%(死亡风险比为0.64;95%CI为0.50至0.81;P<0.001)、50.4%和40.4%(风险比为0.67;95%CI为0.54至0.84;P<0.001),54.4%和44.6%(风险比为0.61;95%CI为0.44至0.84;P=0.001)。最常见的3至5级不良事件是贫血(派姆单抗组为30.3%,安慰剂组为26.9%)和中性粒细胞减少症(分别为12.4%和9.7%)。
由此可见,在同时接受联合或不联合贝伐珠单抗化疗的持续性、复发性或转移性宫颈癌患者中,派姆单抗组的无进展生存期和总生存期显著长于安慰剂组。
原始出处:
Nicoletta Colombo,et al.Pembrolizumab for Persistent, Recurrent, or Metastatic Cervical Cancer.NEJM.2021.https://www.nejm.org/doi/full/10.1056/NEJMoa2112435
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#转移性宫颈癌#
63
#复发性#
75
#持续性#
87
#派姆单抗#
103
#转移性#
61
#宫颈#
70
学习了
175
学习了
75
不错,学习了
128