Sci Rep:NASH炎症机制得到进一步阐明
2017-10-13 佚名 MedSci原创
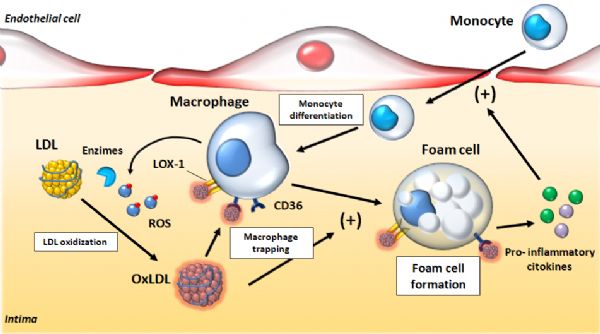
非酒精性脂肪性肝炎(NASH)是与酒精无关的常见肝脏疾病,特征是脂肪在肝脏中积聚,并发生炎症和纤维化。全球NASH病例数持续上升,在中国,一些地区的NASH流行率可高达27%。在美国,NASH患者人数也高达1600万。NASH在没有得到有效治疗的情况下可能会诱发严重的肝脏问题,甚至肝癌。但该疾病的炎症方面的机制仍然未知。近日,欧洲多家研究机构的科学家合作在《Scientific Reports》上
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASH#
87
henhao
92
非常好的文章.学习了.很受益
90
好好学习天天学习
88
不错的.学习了.谢谢分享!
101