Int J Cardiol:阿托伐他汀联合替卡格雷防止缺血再灌注诱导的血管内皮功能障碍!
2017-12-25 xing.T MedSci原创
由此可见,慢性阿托伐他汀结合替卡格雷治疗可以预防急性前臂缺血后血管内皮功能障碍。单独服用替卡格雷可减轻内皮依赖性FBF反应损伤,相比于无药物干预的情况。
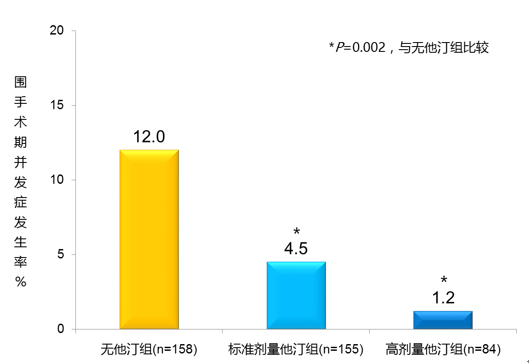
在动物上阿托伐他汀和替卡格雷已被证实可以防止组织损伤。目前还不清楚这些有益的效果是否也能在人类身上重现。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员分析了大剂量阿托伐他汀联合替卡格雷对前臂血管缺血再灌注(IR)损伤模型中内皮功能的影响。
32名健康受试者(每组n=16人)参加了这项随机、安慰剂对照、双盲试验。前臂血流量(FBF)指标随着血管舒张剂乙酰胆碱(Ach;内皮依赖性舒张剂)和硝酸甘油(GTN;内皮非依赖性舒张剂)的血管内剂量增加而增加,这些指标分别在袖带诱导前臂缺血20min前后分别进行测量。研究人员对FBF反应性进行了评估,并且先于任何药物干预前以及在每天一次摄入80mg阿托伐他汀或安慰剂14天后,随后是口服180mg负荷剂量的替卡格雷。此外,还对脂蛋白参数和血小板聚集情况进行了评估。
研究人员发现替卡格雷负荷可以减轻缺血引起的内皮功能障碍,并且联合重复的阿托伐他汀,再灌注期间对ACh的反应完全正常(缺血前后FBF AChAUC比值为0.81[替卡格雷] vs. 1.04 [阿托伐他汀+替卡格雷];P=0.001)。正如预期所想,GTN诱导的血管舒张功能不受IR损伤的影响。阿托伐他汀可显著降低总胆固醇和低密度脂蛋白胆固醇浓度,而高密度脂蛋白胆固醇和甘油三酯水平保持不变。
由此可见,慢性阿托伐他汀结合替卡格雷治疗可以预防急性前臂缺血后血管内皮功能障碍。单独服用替卡格雷可减轻内皮依赖性FBF反应损伤,相比于无药物干预的情况。
原始出处:
Stefan Weisshaar, et al. Atorvastatin combined with ticagrelor prevent ischemia-reperfusion induced vascular endothelial dysfunction in healthy young males – A randomized, placebo-controlled, double-blinded study.International Journal of Cardiology.2017. https://doi.org/10.1016/j.ijcard.2017.12.067
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cardiol#
62
#血管内皮功能障碍#
81
#内皮功能障碍#
92
#血管内皮功能#
74
学习了.谢谢分享
101
#替卡格雷#
72
#功能障碍#
68
#内皮功能#
88
学习了.谢谢分享
104
不错的文章值得推荐
86