Neurology:帕金森病患者前额叶皮质血氧水平依赖性(BOLD)变异性反映环境适应应变性和习得稳定性有限
2022-01-08 Naomi MedSci原创
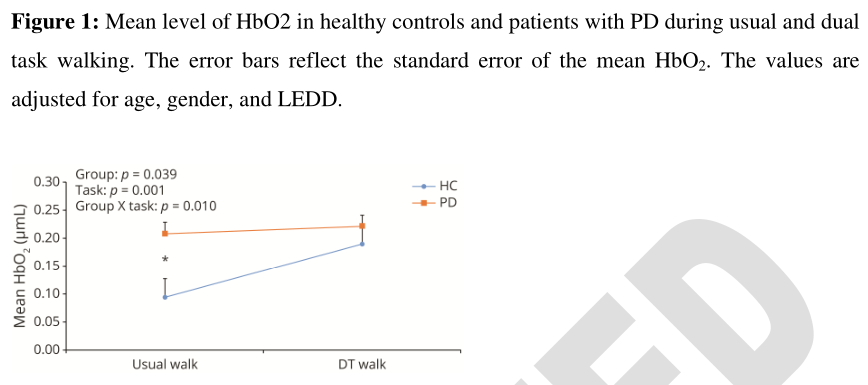
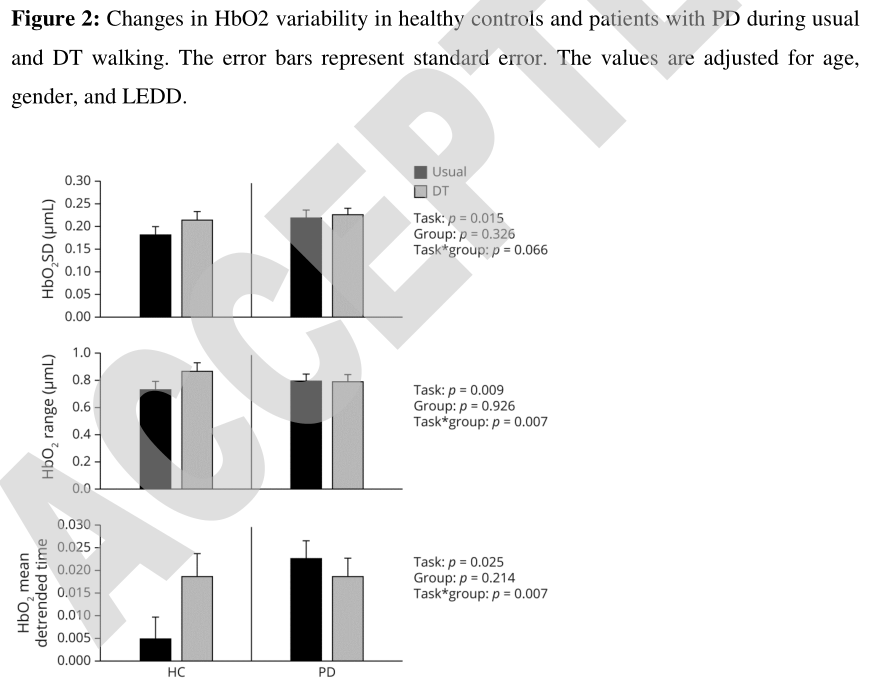
近日,研究人员通过比较普通行走和双任务行走评估任务难度对HBO2变异性的影响,将增加的HBO2变异性与对环境挑战的灵活适应、降低的HBO2变异性与性能的稳定性联系起来。结果表明,两个概念在PD作用有限
越来越多的证据表明,前额叶皮质(PFC)在行走过程中起着重要作用,主要参与计划、组织、执行和对环境的调整。随着年龄和疾病的增加,步态自动性降低与对执行运动控制(一种补偿形式)的依赖增加密切相关。近年来,功能性近红外光谱(FNIRS)对步态的研究表明,在有神经疾病的患者中,正常行走时PFC的平均激活水平较高,从而为这种补偿提供了直接证据。然而,在诸如双重任务行走等要求更高的任务中,健康对照组显示出PFC激活的平均水平升高,而患有帕金森氏病(PD)等神经系统疾病的患者则不然。帕金森病患者PFC激活的有限与步态能力下降有关。
FNIRS测量使用光吸收来检测前额叶皮质的血流动力学变化。放置在前额表面的FNIRS电极发送和接收光(波长750到1000 nm),记录穿过头骨的返回光的变化。其背后的理论基础是,刺激会增加局部脑血流量,因为“激活”区域的能量需求更高,从而导致更高的血氧含量。最近的综述、荟萃分析和共识声明强调了FNIRS在确定主动行走过程中血流动力学反应变化方面的效用。迄今为止,大多数FNIRS研究都基于反映FNIRS时间序列平均值的PFC活动的平均水平。然而,这种方法忽略了新出现的概念,这些概念表明神经激活是一个本质上可变的系统,这种可变性可能揭示对大脑功能的重要见解。最近的研究表明,神经元的可变性是大脑功能的一个重要组成部分,它反映了发育、衰老、疾病状态、任务表现和药理干预。这些研究认为,时间信号的可变性是量化神经成像时间序列中时刻变化幅度的一种量度。这种可变性的两种简单形式是:范围,表示数据在分布中从最低值到最高值的分布;标准差(SD),反映测量的总体分布宽度。平均下降趋势时间序列是一种额外的、稍微复杂的变异性形式。
功能磁共振成像研究显示,随着年龄的增长,皮质区域的血氧水平依赖性(BOLD)变异性降低,而皮质下区域(如纹状体)的BOLD变异性增加。此外,BOLD变异性指标在预测年龄方面显示出比中心倾向指标(如平均数)更强大的能力,与更年轻人群相比,健康对照组在任务中表现出的变异性较少,这表明这些指标包含的重要信息。此外,在认知任务中表现更好的参与者表现出更高的大脑信号可变性,这表明神经处理的可变性实际上可能是有益的,潜在地反映了灵活性。研究还显示,从休息到任务,BOLD的变异性会增加,并且与任务难度有关。这进一步表明,大脑信号的变异性在神经系统适应变化的环境或在某些情况下保持稳定的能力中起着重要作用。适应性和灵活性的这些方面大多是在前额神经网络的背景下报道的,前额神经网络在不同的行为情况下表现出不同的可变性,需要灵活性或稳定性。在包括任务重复的练习中,需要较低的可变性来适应和保持特定的任务目标,而要灵活地切换到不同的任务,则需要较高的可变性。因此,稳定和灵活的行为对于日常生活中的成功行走至关重要。
最近的一项研究表明,使用FNIRS的老年人在日常行走和双重任务行走过程中,个体内PFC变异性发生了变化。计算每个步行任务的FNIRS衍生氧合血红蛋白(HBO2)测量的标准差(SD),并在任务和认知能力改变的参与者之间进行比较。与更简单的步行条件相比,在双重任务步行条件下,变异性增加。此外,与那些没有认知障碍的人相比,有认知障碍的老年人在不同任务间增加的变异性更大。帕金森病患者在进行双重任务时走路的研究表明,双重任务对行走性能的变异性增加了强烈的负面影响。然而,FNIRS在帕金森病患者中的HBO2变异性尚未得到评估。帕金森病是一种具有明显步态和认知缺陷的神经退行性疾病。
近日,有研究人员通过比较普通行走和双任务行走来评估任务难度对HBO2变异性的影响,并通过比较任务重复之间的差异来评估任务练习对HBO2变异性的影响,以研究与健康对照组比较,研究帕金森病患者步行过程中个体内HBO2变异性的不同方面。其中常规行走和双重任务行走之间的比较能够检查神经灵活性,而任务重复之间的比较则允许检查神经稳定性。
研究共纳入206名受试者,57名健康对照者(年龄:68.9±1.0岁,27名女性)和149名特发性帕金森病患者(年龄:69.8±0.6岁,50名女性,病程:8.27±5.51年)进行常规步行和双任务步行(连续3次减法),额部放置 FNIRS系统。使用在每个步行任务中评估的 FNIRS获得的HBO2信号的标准差(SD)、范围和平均去趋势时间序列来计算HBO2变异性。使用混合模型分析比较不同组之间和不同步行任务之间的HBO2变异性。
- 双任务步行时的变异性(SD、极差、平均去趋势时间序列)高于平时步行(P<0.025),但这是由于健康对照组内部的差异(X组任务交互作用:P<0.007)。
- 在健康对照组中,任务重复显示变异性降低,而在帕金森病患者中,变异性增加(互动组*步行-重复:P<0.048)。
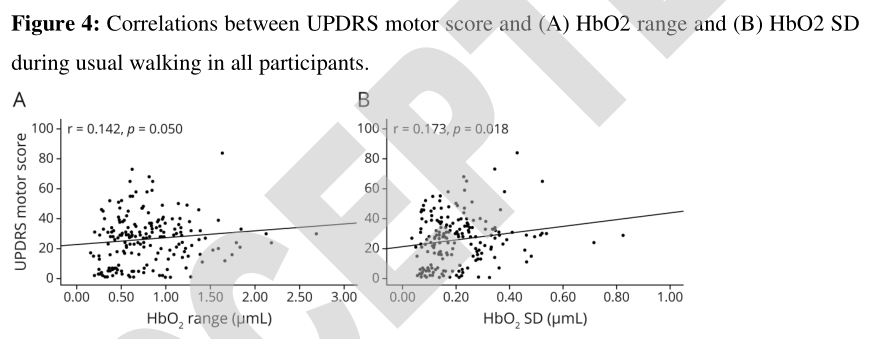
- 所有受试者的MDSUPDRS运动评分与平时步行时的HBO2范围(r=0.142,p=0.050)和HBO2 SD(r=0.173,p=0.018)呈正相关。
这项研究提出了一种新的方法来解释HBO2变异性的变化,将增加的HBO2变异性与对环境挑战的灵活适应联系起来,将降低的HBO2变异性与性能的稳定性联系起来。结果表明,这两个概念在PD中都是有限的,但这些概念还需要进一步的研究。此外,HBO2变异性测量是大脑功能的一个重要方面,它为PFC在衰老和帕金森氏症步行过程中的作用提供了新的见解。
这项研究提供了Ⅲ类证据,表明帕金森病患者在平时步行时,与健康对照组相比,Hb02信号有更多的变异性,但在双重任务步行时没有变化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#稳定性#
107
#帕金森病患者#
126
#Neurol#
93
#变异#
81
#变性#
97
#血氧#
96
#帕金森病患#
115