ACC 2016:女性可通过钼靶筛查识别早期心血管风险
2016-03-25 Seven L MedSci原创
在芝加哥举行的第65届美国心脏病学会科学会议称,常规钼靶可识别女性的心脏病风险,进行更早期的干预。研究成果将于4月4日发表在JACC: Cardiovascular Imaging。Laurie Margolies博士和同事对292名行钼靶和CT的女性进行了一项研究,探究乳房动脉钙化(BAC)和冠状动脉钙化(CAC)的关系。研究数据显示,BAC存在于42.5%的女性中,这类女性中有70%的伴有CA
在芝加哥举行的第65届美国心脏病学会科学会议称,常规钼靶可识别女性的心脏病风险,进行更早期的干预。研究成果将于4月4日发表在JACC: Cardiovascular Imaging。
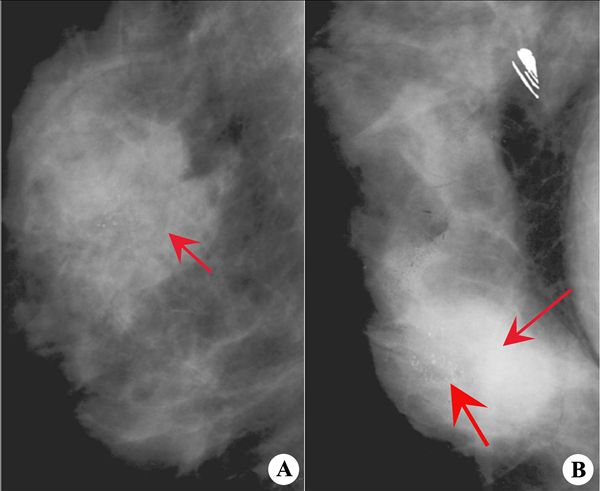
Laurie Margolies博士和同事对292名行钼靶和CT的女性进行了一项研究,探究乳房动脉钙化(BAC)和冠状动脉钙化(CAC)的关系。
研究数据显示,BAC存在于42.5%的女性中,这类女性中有70%的伴有CAC。此外60岁以下女性中有一半的有BAC,更年轻的BAC女性中有83%的伴有CAC。与先前的研究一致,BAC是心血管风险的强预测因素。
研究的共同作者、JACC: Cardiovascular Imaging的总编辑Jagat Narula博士说:“研究表明,我们现在有许多提供关于亚临床冠状动脉疾病信息的数据,本研究中,BAC对亚临床动脉粥样硬化的预测价值等同于标准的危险因素。不过数据并不来自于前瞻性研究,存在选择性偏倚。虽然我们和其他人都观察到了BAC和CAC之间的联系,但是血管的钙化机制却不同,期间的直接联系我们也不知道。不过当你发现有能预测亚临床冠状动脉疾病信息的数据,就应该提高警觉。”
另外Amorina Ishai博士和同事对293名进行PET/CT扫描后发现,大脑压力中心活动度越大,心血管事件风险越高,活动度每增加1U,风险增加14倍。超过5年的随访发现,高压和低压参与者相比,心血管事件发生率分别为35%和15%。
作者指出,以后还需要更多的研究去探究压力与心血管事件的关系,通过降低大脑压力中心的活动度,能否减少动脉粥样硬化相关炎症,进而降低心血管事件风险。
原始出处:
Study Finds Routine Mammography May be Useful For Heart Disease Screening.Mar 24, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管风险#
47
#ACC#
55
需要进一步的研究证实
100
谢谢分享。
175
是这样吗
165
要多看文献
75