点击下方链接查看指南原文
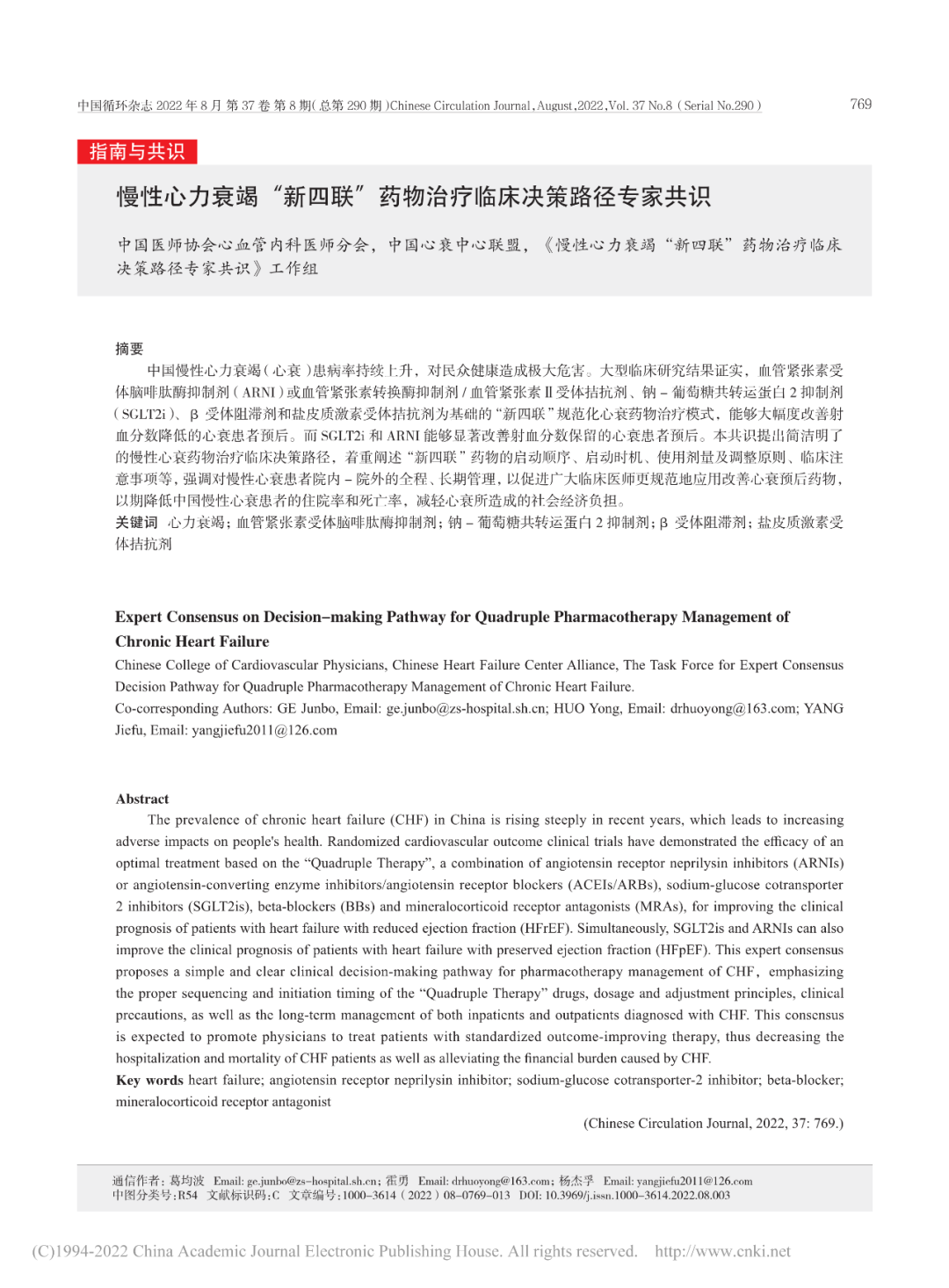
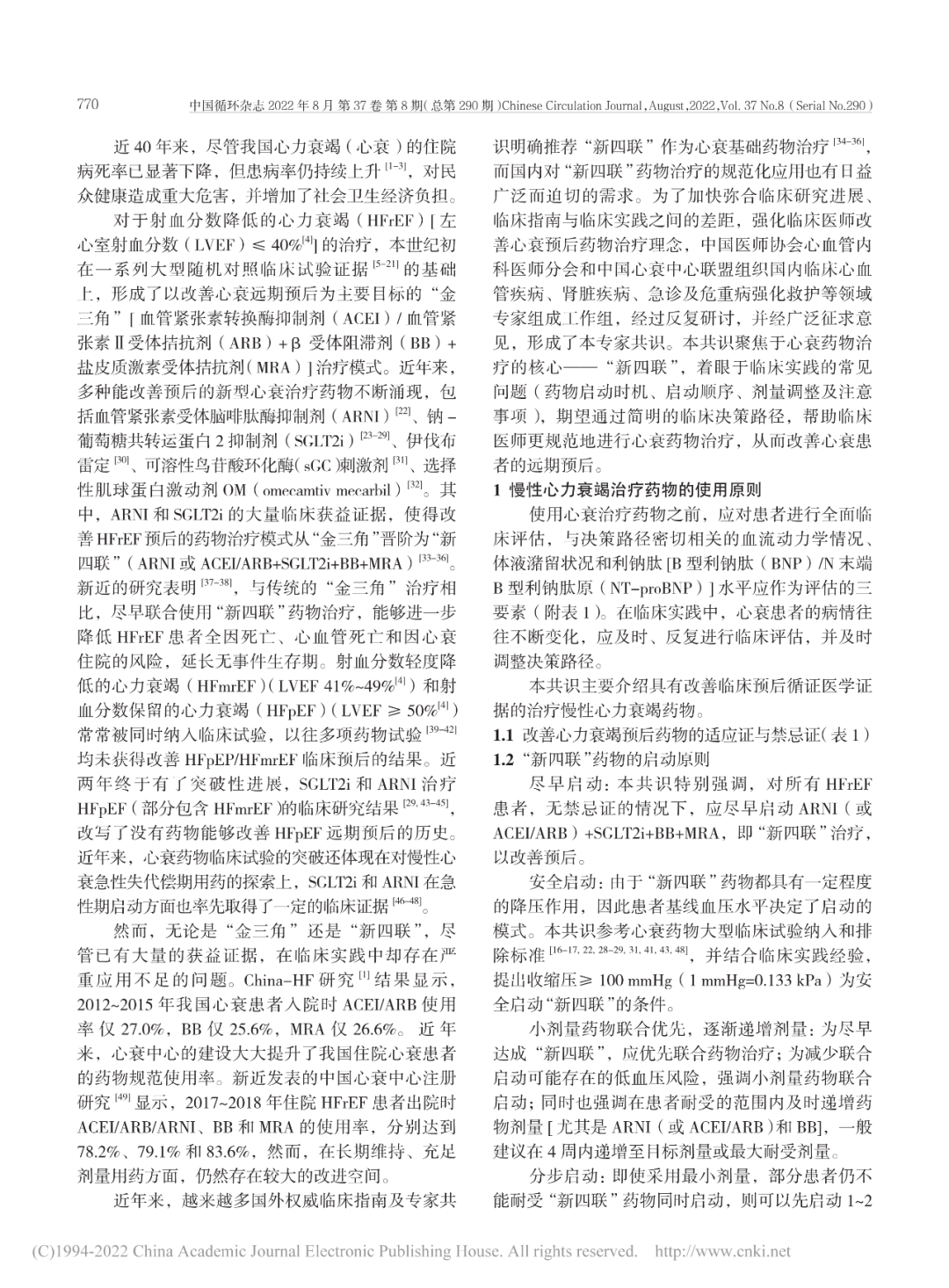
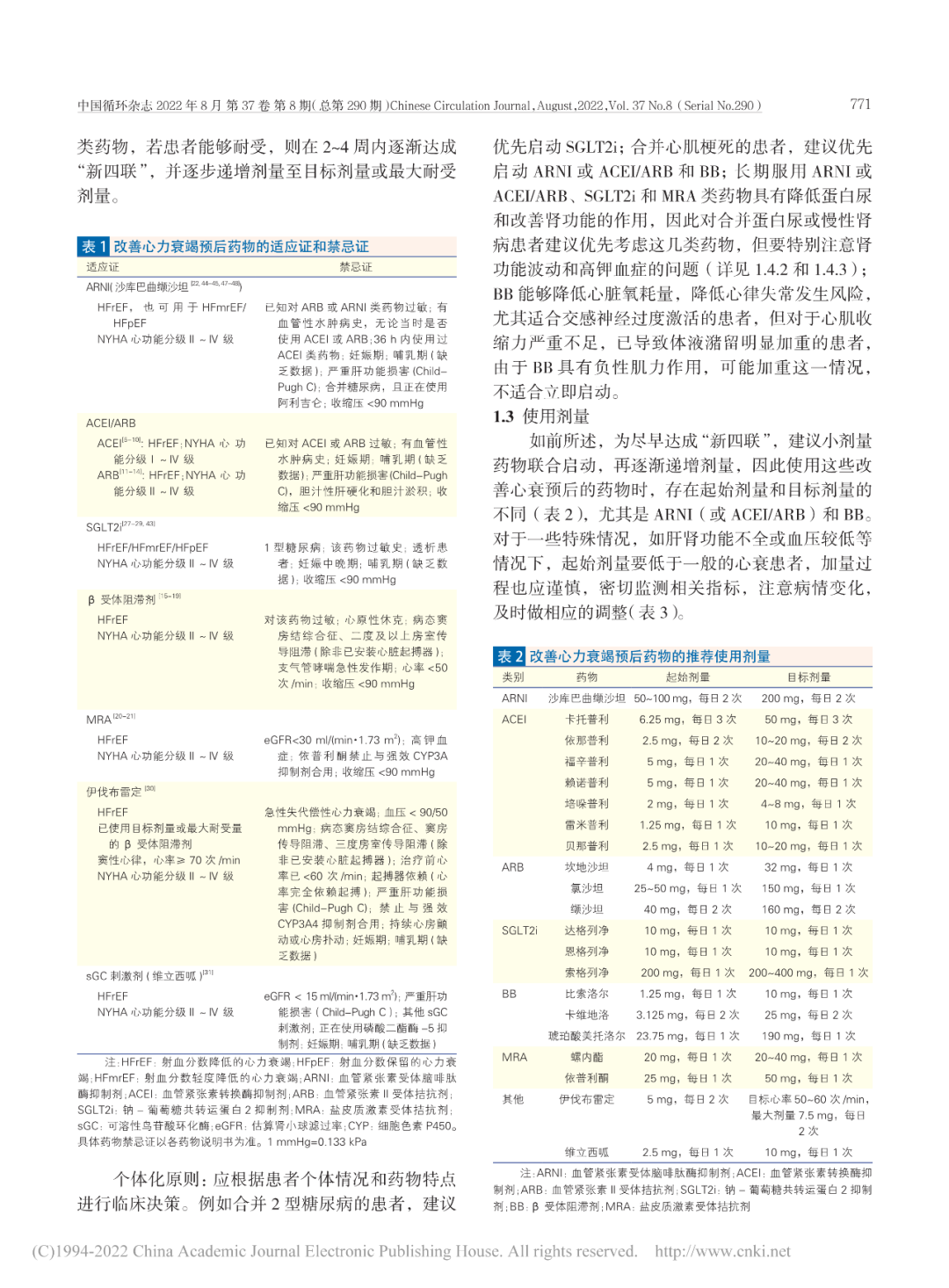
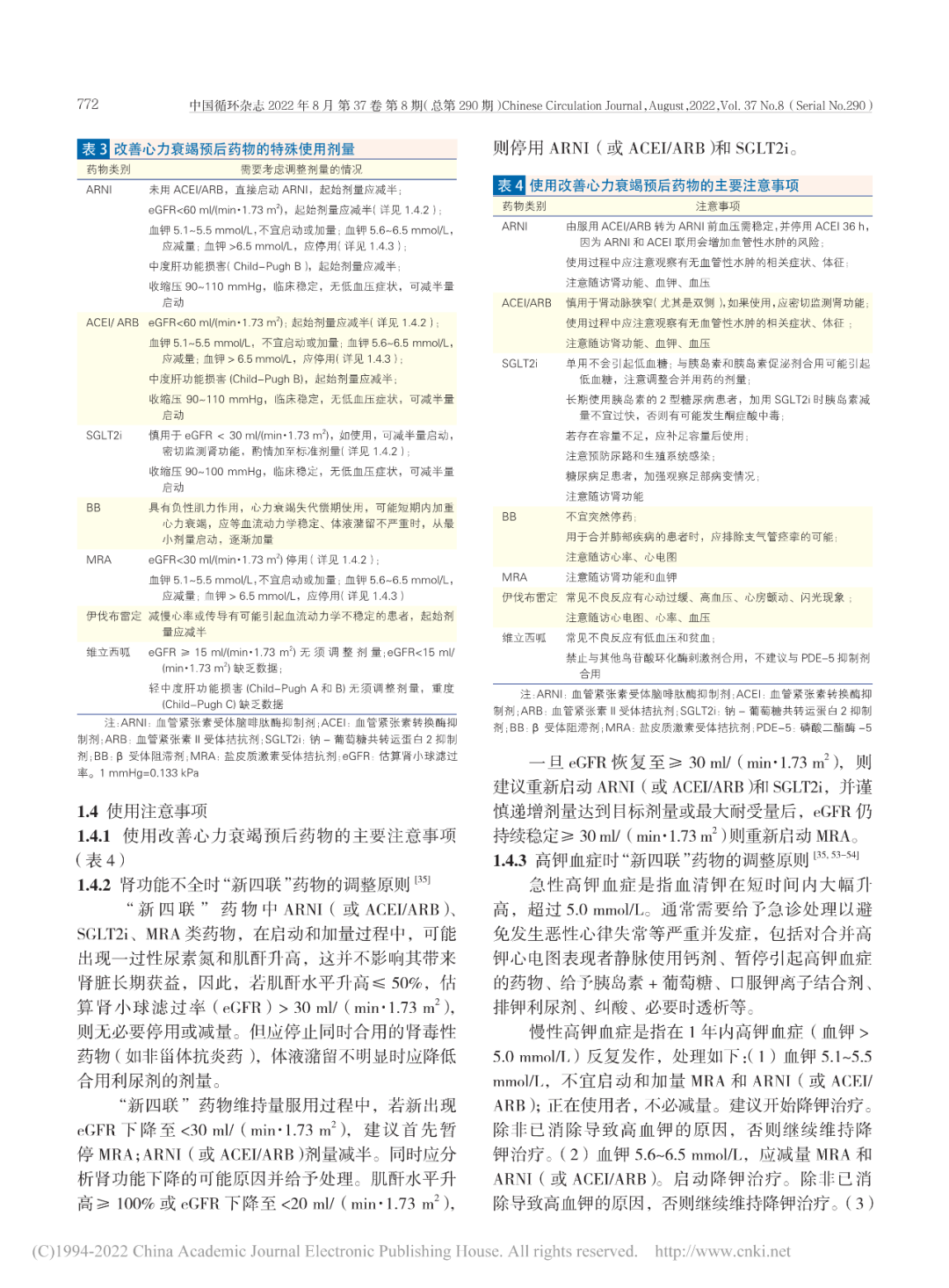
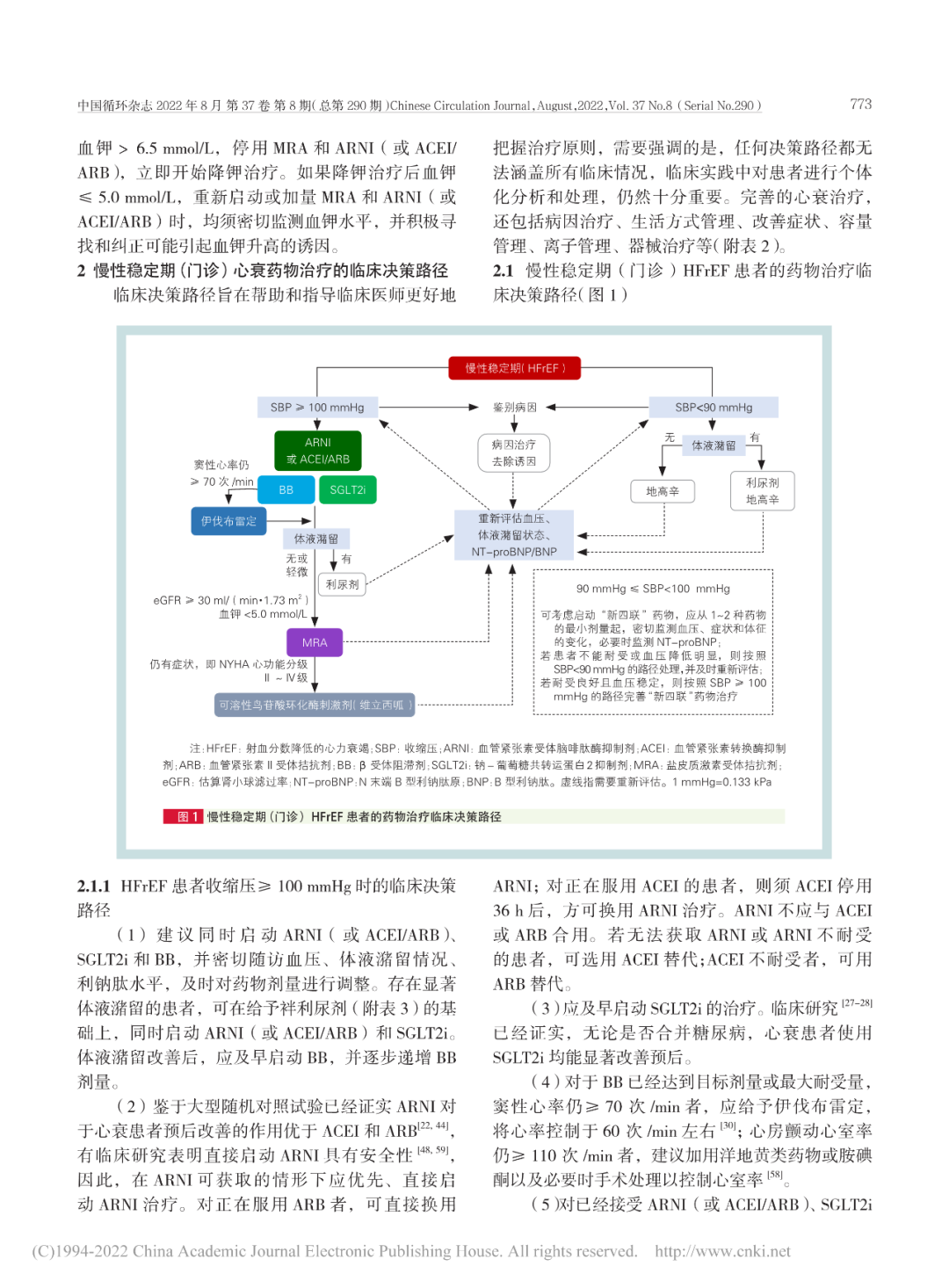
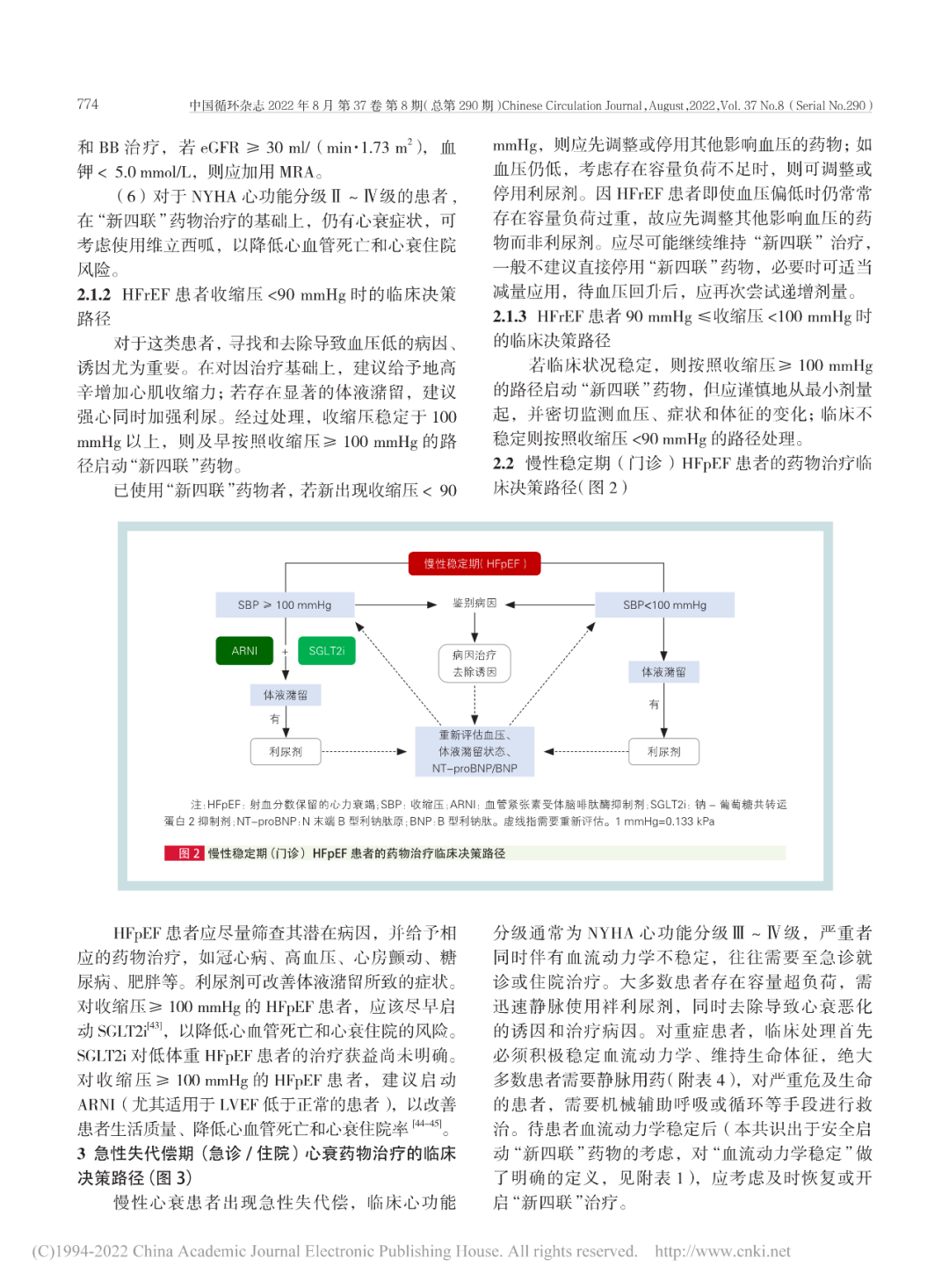
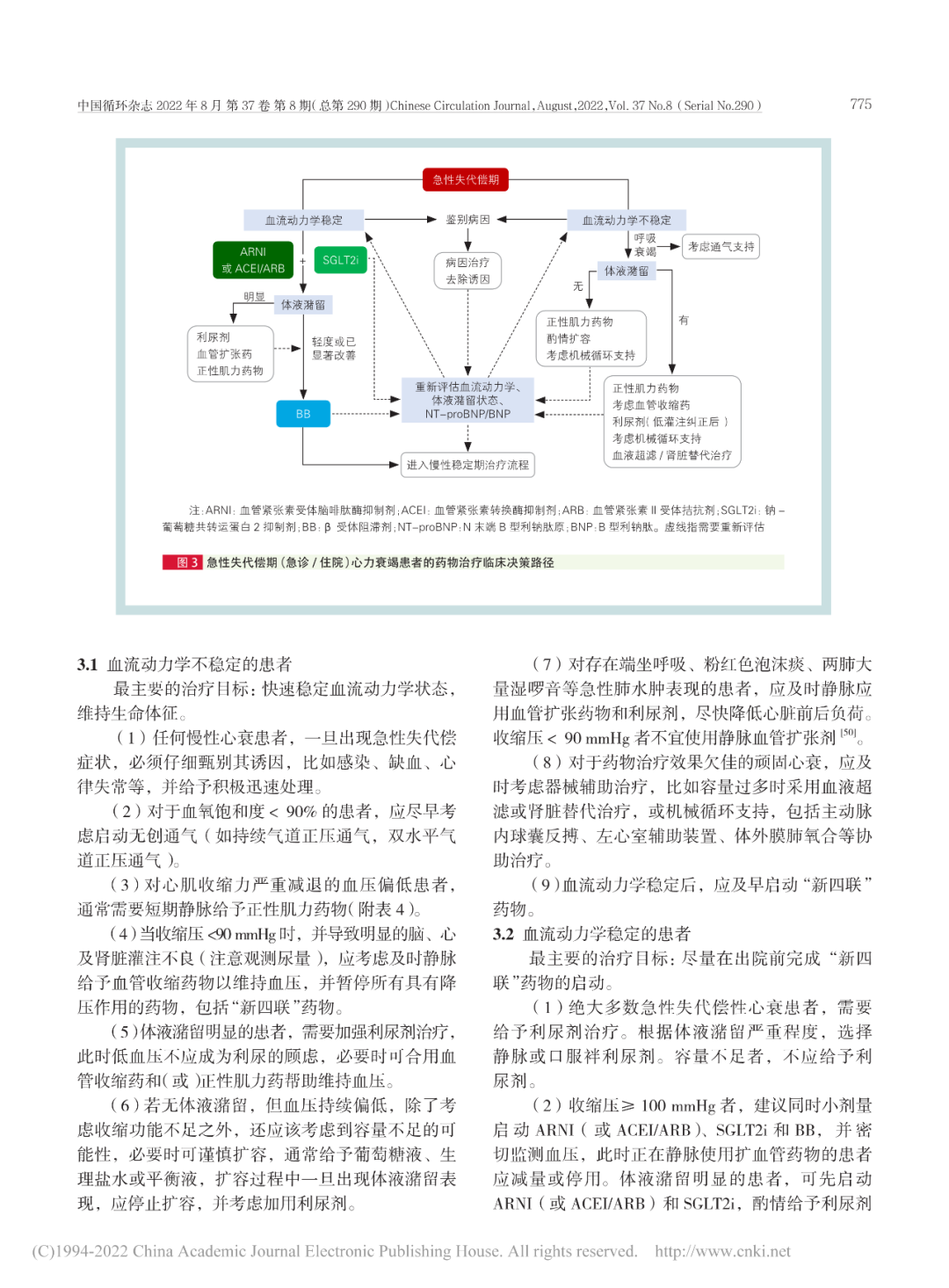
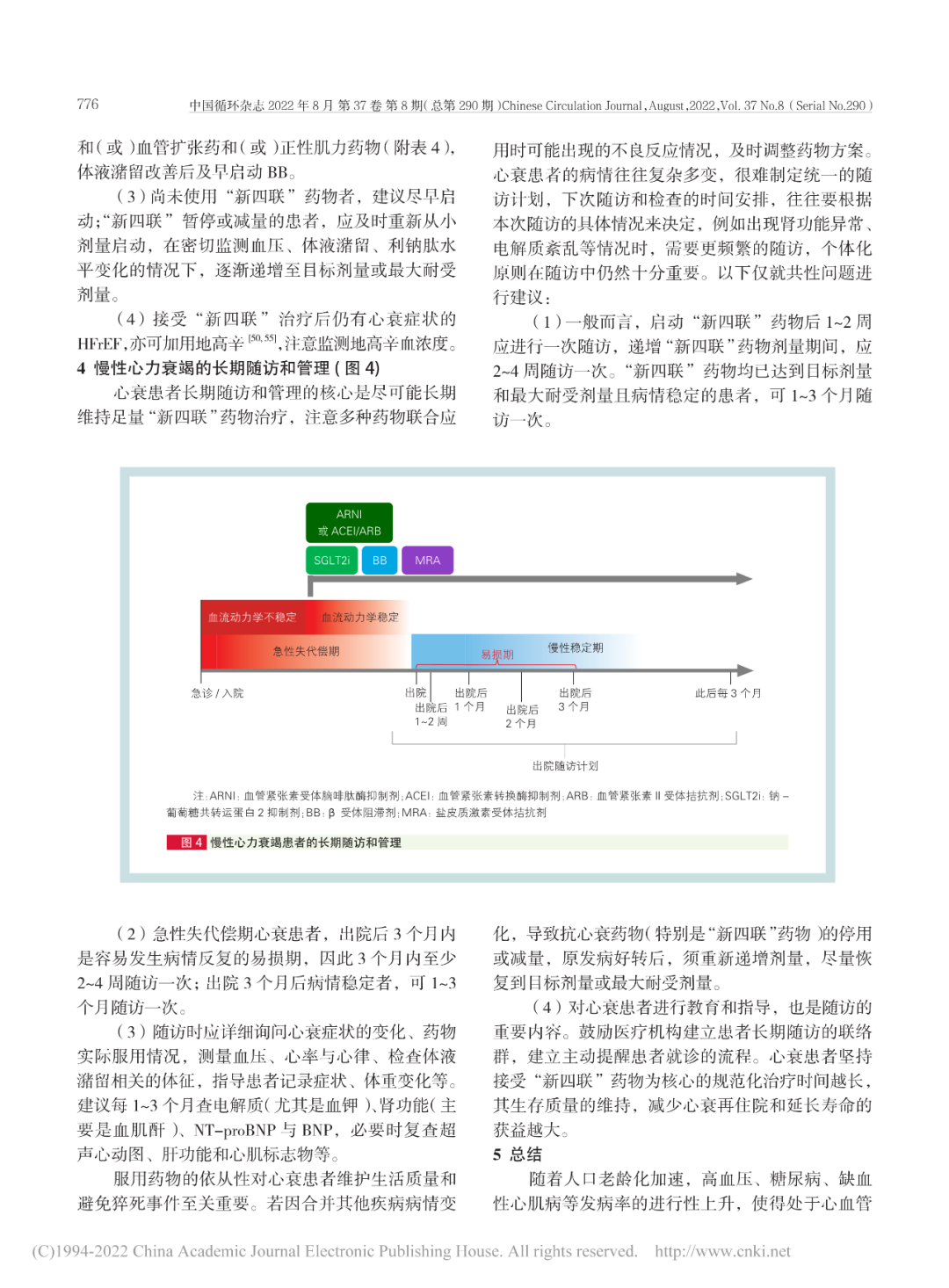
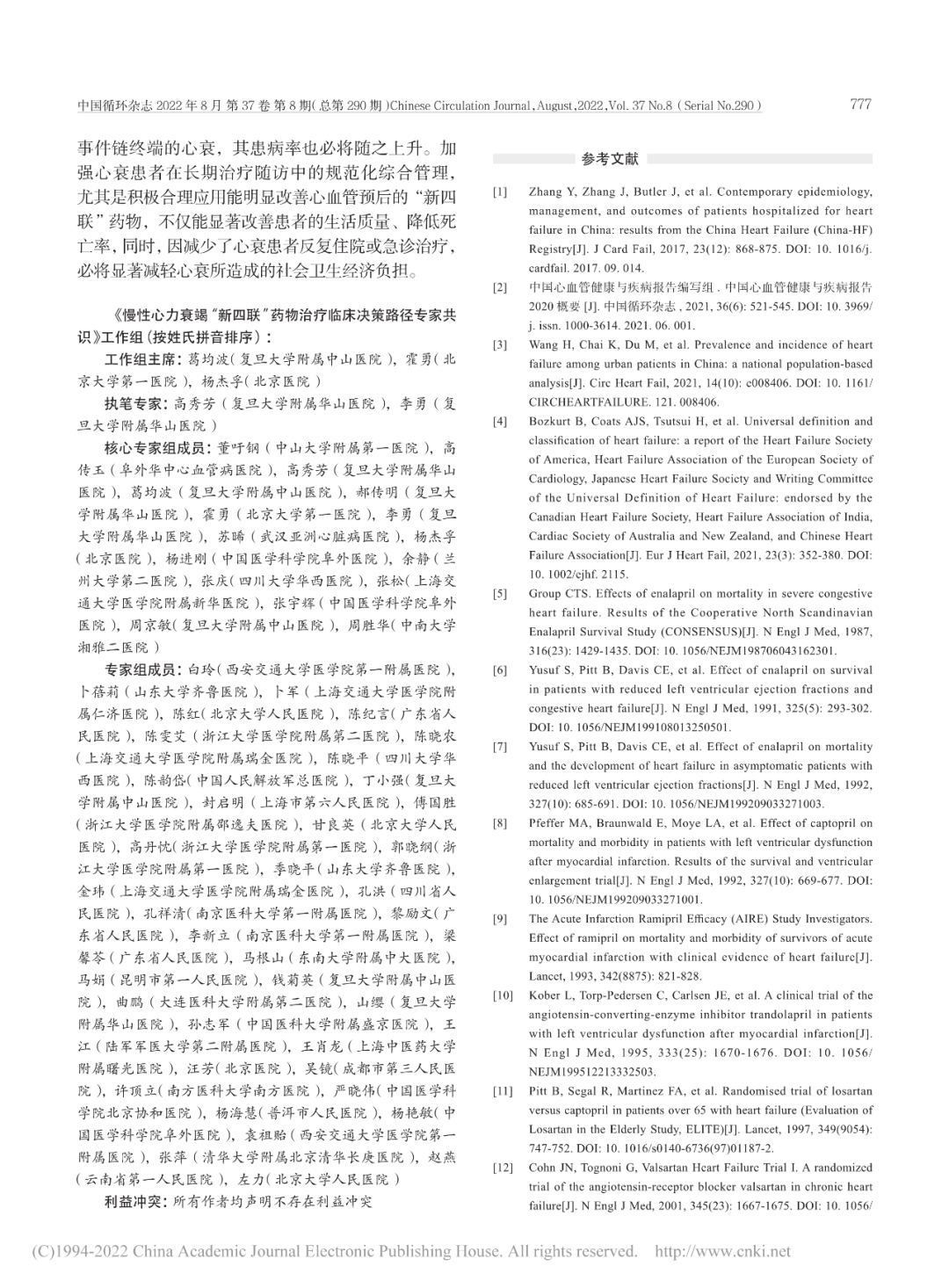
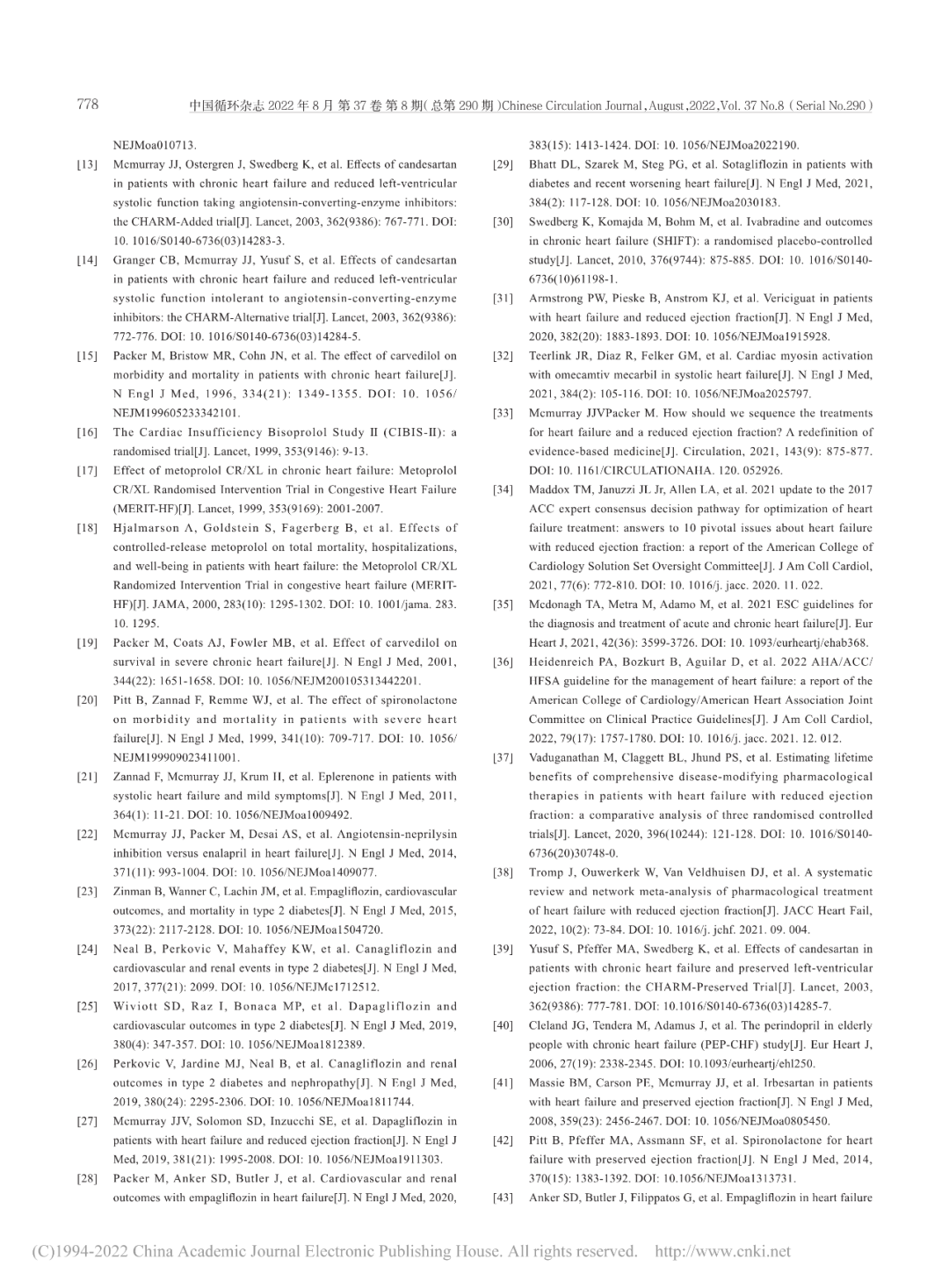
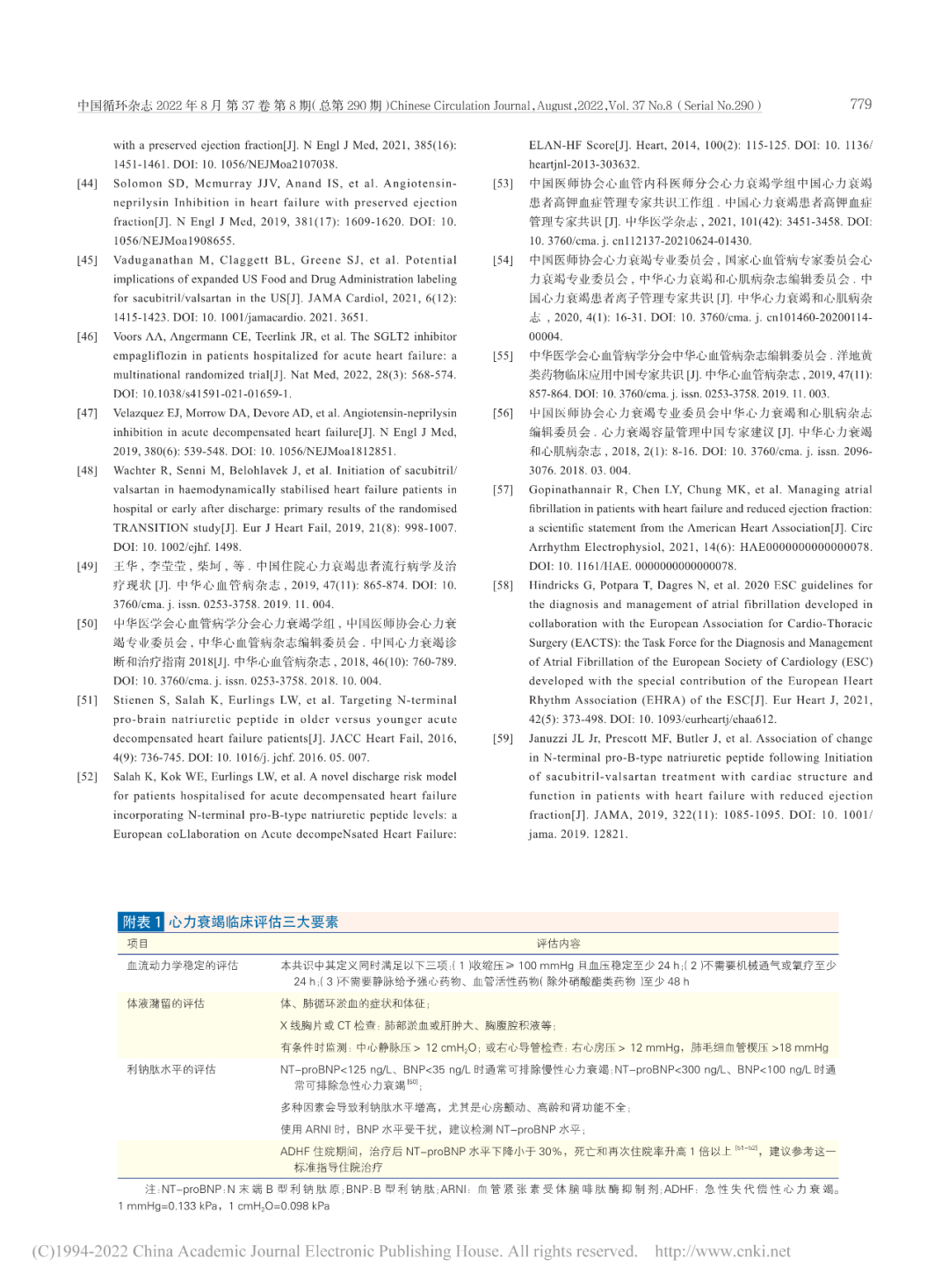
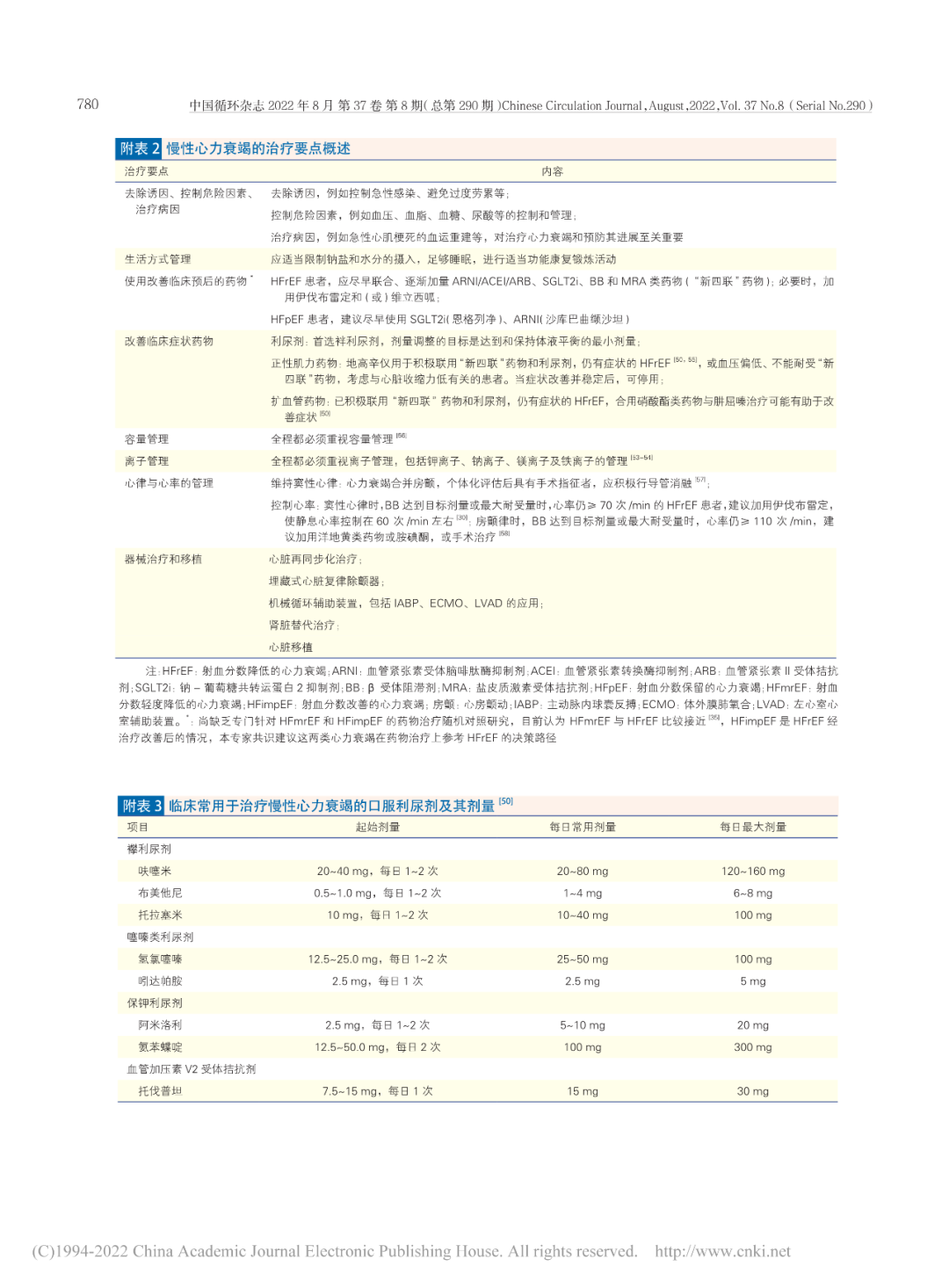
中国慢性心力衰竭(心衰)患病率持续上升,对民众健康造成极大危害。大型临床研究结果证实,血管紧张素受体脑啡肽酶抑制剂(ARNI)或血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体拮抗剂、钠-葡萄糖共转运蛋白2抑制剂(SGLT2i)、β受体阻滞剂和盐皮质激素受体拮抗剂为基础的“新四联”规范化心衰药物治疗模式,能够大幅度改善射血分数降低的心衰患者预后。而SGLT2i和ARNI能够显著改善射血分数保留的心衰患者预后。
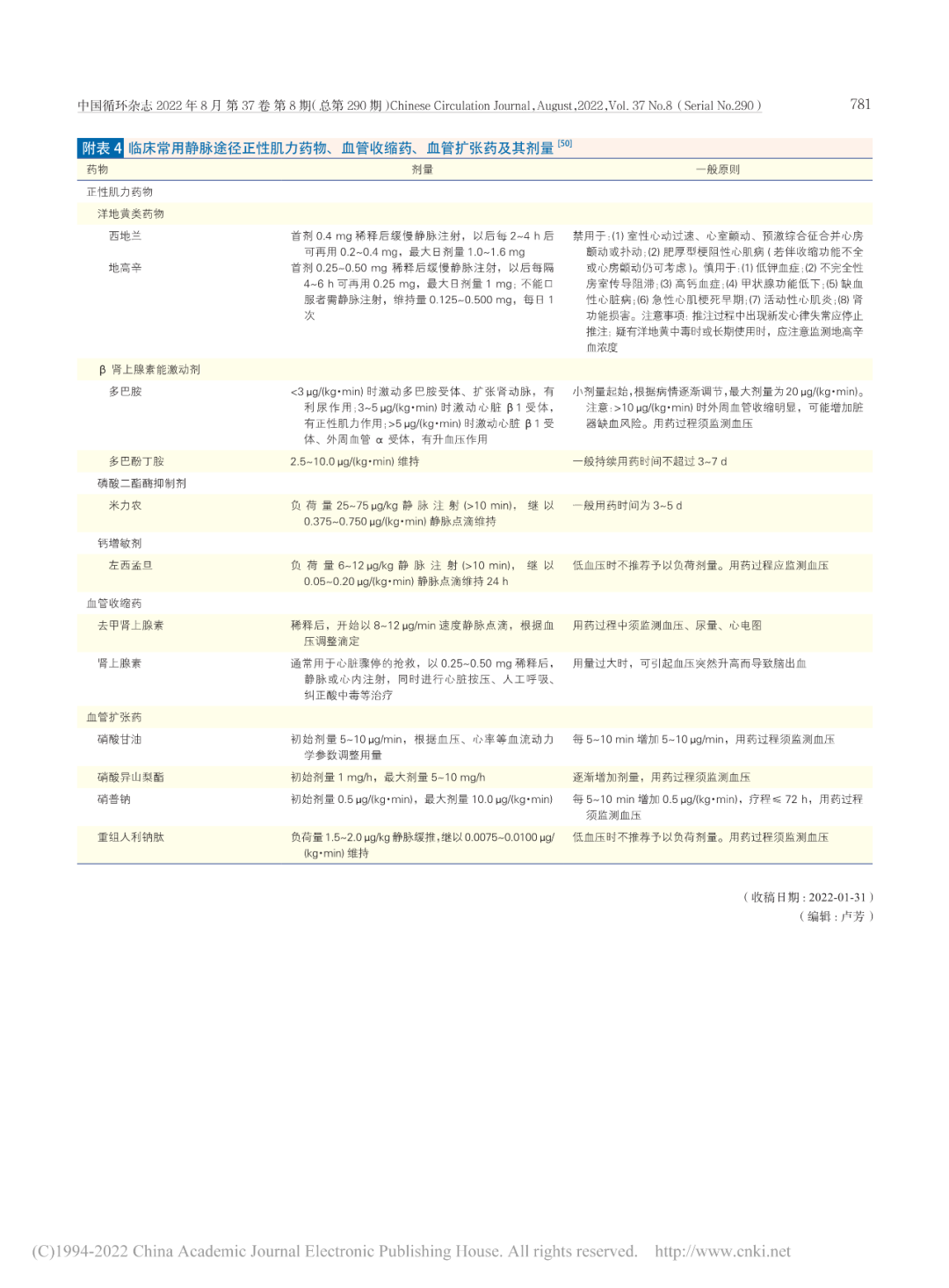
本共识提出简洁明了的慢性心衰药物治疗临床决策路径,着重阐述“新四联”药物的启动顺序、启动时机、使用剂量及调整原则、临床注意事项等,强调对慢性心衰患者院内-院外的全程、长期管理,以促进广大临床医师更规范地应用改善心衰预后药物,以期降低中国慢性心衰患者的住院率和死亡率,减轻心衰所造成的社会经济负担。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#临床决策#
105
#专家共识#
119
#慢性心力衰竭#
117
#决策#
112
好!
83
写的真好!
100