Rheumatology (Oxford):脂肪组织来源的基质血管用于治疗系统性硬化症患者的效果如何?
2022-07-02 MedSci原创 MedSci原创
系统性硬化症(SSc)是一种罕见的自身免疫性疾病,其特点是纤维化过程和周围血管病变,损害许多器官的功能。从日常的生活质量和职业的角度来看,最常见的是手部残疾。
系统性硬化症(SSc)是一种罕见的自身免疫性疾病,其特点是纤维化过程和周围血管病变,损害许多器官的功能。从日常的生活质量和职业的角度来看,最常见的是手部残疾。近日,发表于Rheumatology (Oxford)的一项研究评估向手指注射脂肪组织来源的基质血管部分(AD-SVF)与安慰剂相比在减少SSc患者的手部残疾方面的优越性。

研究人员于2015年10月至2018年1月在法国进行了一项双盲、多中心、II期试验。将CHFS≥20/90的SSc患者按1:1随机接受注射AD-SVF或安慰剂。AD-SVF是使用自动处理的Celution 800/CRS系统获得的。安慰剂是乳酸林格氏液。主要疗效终点是CHFS评分从基线到3个月的变化。次要疗效终点包括6个月时的CHFS评分、手部功能、血管病变、手部疼痛、皮肤纤维化、指浆敏感性、硬皮病健康评估问卷、患者和医生满意度以及安全性。
结果,共随机分组40名患者。AD-SVF组和安慰剂组在年龄、性别比例、病程、手部皮肤纤维化和手部残疾的主要原因方面具有可比性。经过3个月的随访,两组的手部功能都有明显改善,CHFS没有组间差异(AD-SVF组的平均变化为-9.2[12.2],安慰剂组为-7.6[13.2])。6个月时,两组的手部功能都有改善。
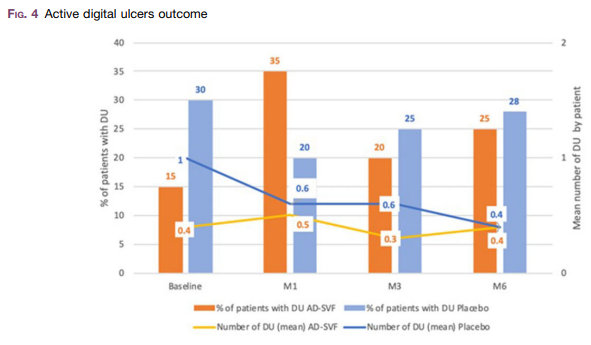
综上所述,该研究结果表明,随着时间的推移,两组的手部功能都有改善,AD-SVF治疗没有额外的优势。考虑到本试验的局限性,应鼓励对更多具有同质表型和手部障碍的患者进行研究,以准确评估AD-SVF治疗的益处。
原始出处:
Aurélie Daumas, et al., Adipose tissue-derived stromal vascular fraction for treating hands of patients with systemic sclerosis: a multicentre randomized trial Autologous AD-SVF versus placebo in systemic sclerosis. Rheumatology (Oxford). 2022 May 5;61(5):1936-1947. doi: 10.1093/rheumatology/keab584.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Rheumatology#
115
#硬化症#
134
#系统性#
106
#基质#
100
#Oxford#
89
认真学习~~
97
#脂肪组织#
114
#系统性硬化#
152