AASLD 2017:范建高教授点评:HepQuant-STAT简易肝功能定量检测对NASH的无创诊断与评估
2017-10-23 佚名 国际肝病
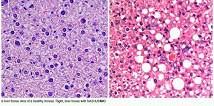
非酒精性脂肪性肝炎(NASH)的诊断金标准为肝脏病理活检,但因其有创性与采样误差而应用受限。第68届美国肝病研究学会(AASLD)年会口头报告平行会上,来自美国的研究团队报道了一种简易肝脏功能定量检测——HepQuant-STAT(HQ-STAT),其可无创诊断非酒精性脂肪性肝炎(NASH),并评估疾病严重程度(摘要号:96)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#无创诊断#
93
#AASLD#
77
#ASH#
66
#肝功能#
79
#ASL#
70