DCR: IBD患者全结肠切除术后直肠癌的发生风险明显降低
2021-04-17 MedSci原创 MedSci原创
与普通人群相比,IBD患者罹患结直肠癌(CRC)的风险明显增加,在IBD诊断后的25年内,几乎三分之一的结肠IBD患者会经历严重的疾病复发,需要进行结肠切除术。
与普通人群相比,IBD患者罹患结直肠癌(CRC)的风险明显增加,在IBD诊断后的25年内,几乎三分之一的结肠IBD患者会经历严重的疾病复发,需要进行结肠切除术。通常来说接受结肠切除术的患者相对较年轻,并且患有广泛的病变,因此,接受IBD全结肠切除术的患者可能在直肠残余物中罹患癌症的风险更高。因此,本项研究旨在评估IBD全结肠切除术后直肠癌的风险。

研究人员收集了1977年至2013年在丹麦进行了全结肠切除术的IBD患者的临床资料。通过长期随访了解了IBD和全结肠切除术患者中直肠癌的发生率,并将其与丹麦其他直肠癌患者的癌症分期进行了比较。使用Kaplan-Meier方法估算了直肠癌诊断后的生存率,并使用Cox回归估算了调整后的死亡率。
本项研究共纳入了4703例IBD患者(1026克罗恩氏病; 3677溃疡性结肠炎),所有患者均接受了全结肠切除术并伴有直肠残留。在29725年的随访期间,研究人员总共观察到30例直肠癌的发生,而预期直肠癌发病数为8(OR= 3.6(95%CI,2.4-5.1))。全结肠切除术后35年直肠癌的风险为1.9%(95%CI,1.1%-2.9%)。直肠癌诊断五年后,IBD患者并有直肠残留的患者的生存率要高于非IBD患者38% VS 28%(P=0.001)
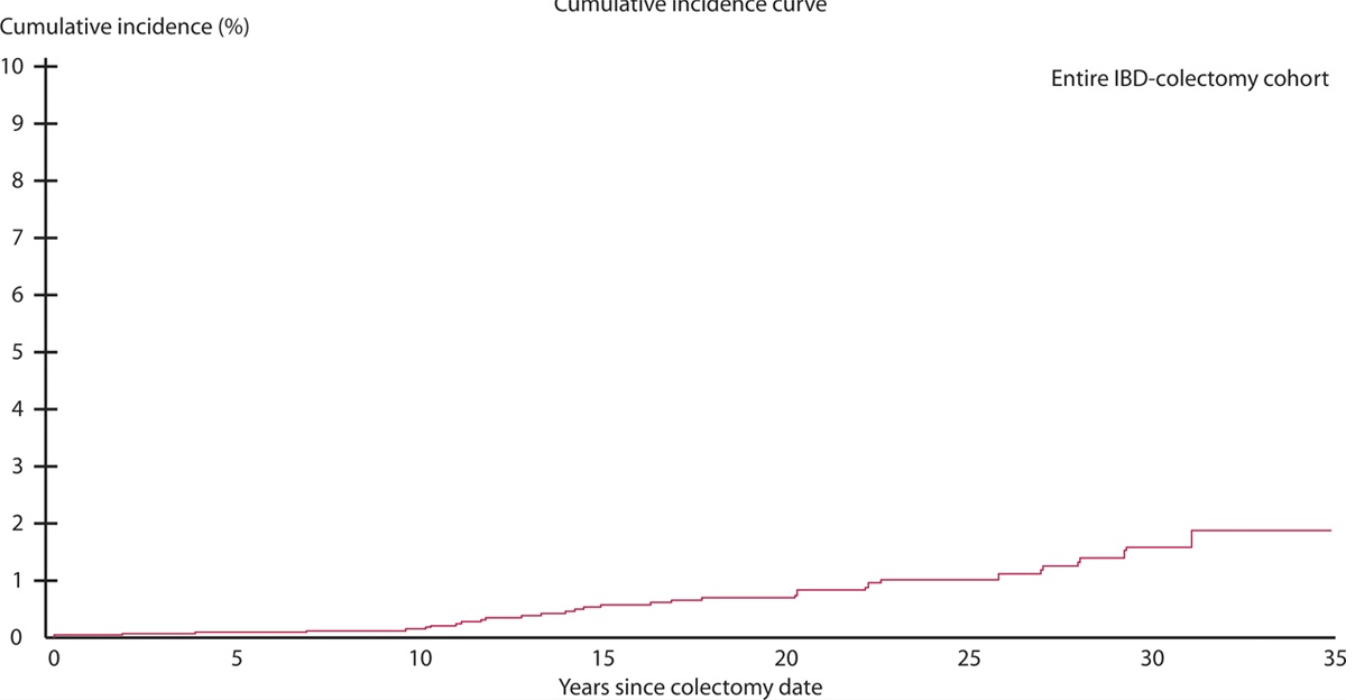
图:全结肠切除对于IBD患者生存率的影响
本项研究证实IBD患者行全结肠切除术后直肠癌的长期风险较低。诊断为直肠癌的IBD行全结肠切除术后生存率明显提高。
原始出处:
Mark-Christensen. Et al. Rectal Cancer Risk and Survival After Total Colectomy for IBD: A Population-Based Study. Diseases of the Colon & Rectum.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#结肠切除术#
85
#切除术#
64
好的吧
100
哦哦哦哦哦哦
96
#IBD#
72