Eur J Heart Fail:左心房功能指标可预测低风险人群心衰
2021-12-22 MedSci原创 MedSci原创
在一般人群中,LAVImin是发生HF的独立预测因子。LAVImax是目前常规超声心动图检查中唯一的LA测量指标,并非HF发生的独立预测指标。
在全球范围内,心力衰竭(HF)是心血管死亡率和发病率的主要原因。HF在西方国家的患病率约为1-2%,5年死亡率高达35%。

近日,心血管领域权威杂志European Journal of Heart Failure上发表了一篇研究文章,该研究旨在调查通过经胸超声心动图测量的左心房(LA)参数作为社区队列中发生心力衰竭(HF)预测指标的效能。
在这项大型普通人群研究(n=2221)中,参与者接受了超声心动图检查。研究人员测量了参与者与体表面积相关的最大和最小LA容积(LAVImax和LAVImin),并计算LA排空分数(LAEF)和LA扩张指数(LAEI)。
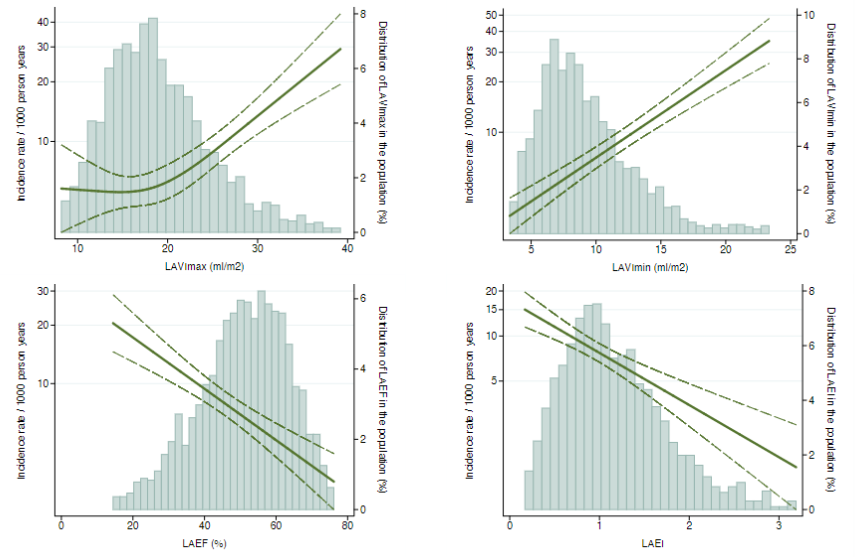
在1951名没有房颤或明显瓣膜疾病的参与者中,平均年龄为59±16岁,58%为女性。在基线时,1%(n=16)的参与者LV射血分数低于50%,44%的参与者患有高血压,10%的参与者患有糖尿病。在随访期间(中位数为15.8年,IQR为11.3-16.2年),187名(10%)参与者被诊断出HF。与没有HF的参与者相比,在随访期间被诊断为HF的参与者具有更大的LAVImax和LAVImin,以及更低的LAEF和LAEI。在未经调整的分析中,LAVImax、LAVImin、LAEF和LAEI是发生HF的预测因子。在对临床和超声心动图参数进行多变量调整后,只有LAVImin仍然是HF发生的独立预测因子(每增加1个SD的HR为1.22(1.01-1.47),p=0.038)。
由此可见,在一般人群中,LAVImin是发生HF的独立预测因子。LAVImax是目前常规超声心动图检查中唯一的LA测量指标,并非HF发生的独立预测指标。
原始出处:
Ditte Madsen Andersen.et al.Measures of Left Atrial Function Predicts Incident Heart Failure in a Low Risk General Population: The Copenhagen City Heart Study.European journal of heart failure.2021.https://onlinelibrary.wiley.com/doi/abs/10.1002/ejhf.2406
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#左心房#
67
#ART#
48
#HEART#
53
#左心房功能#
60
#心房#
58