哈佛大学84万人的研究发现:晚上11点前睡觉,抑郁风险降低40%!
2021-06-01 K.K MedSci原创
早上可以喝杯咖啡。方便的话,步行或骑自行车上班,晚上将电子产品调暗
昼夜偏好已经成为严重抑郁症(MDD)风险的潜在因素,先前的孟德尔随机化研究(MR)发现了昼夜偏好与幸福感和精神分裂症有关的证据,但对严重抑郁症的关联是没有的。5月26日,麻省理工学院和哈佛大学布罗德研究所等研究人员发表在JAMA Psychiatry上的一项约84万人的研究发现:在特定时间里,一个人的某些睡眠倾向可能会导致抑郁症风险。这项MR分析发现了较早的昼夜偏好与较低的MDD风险之间存在保护性关联的有力的证据。
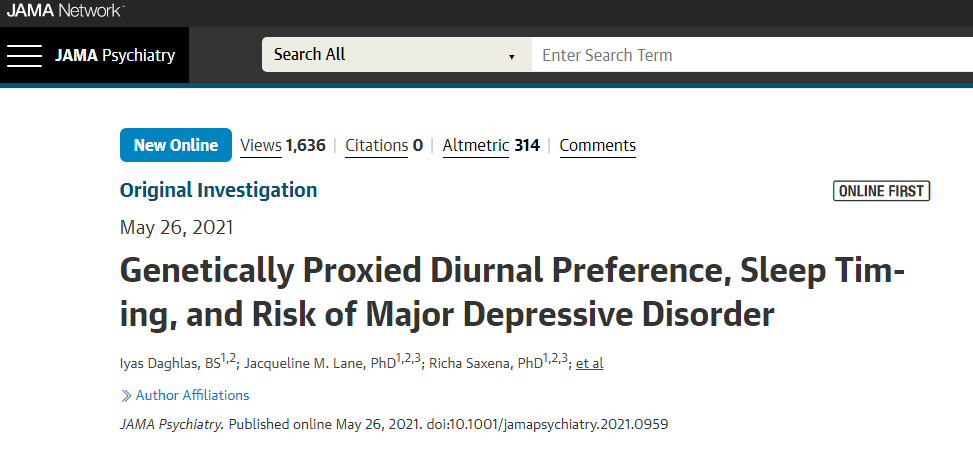
Iyas Daghlas et al, Genetically Proxied Diurnal Preference, Sleep Timing, and Risk of Major Depressive Disorder,JAMA Psychiatry(2021).DOI: 10.1001/jamapsychiatry.2021.0959
研究数据包含英国生物样本库(UKB)、23andMe公司、全基因组关联(GWAS)研究的数据,其中,GWAS中有697828位,23andMe公司有24098位,UKB有85502位。
研究人员发现,遗传学上的昼夜偏好与MDD的风险降低有关。睡眠中点(就寝时间和醒来时间之间)提前0.5小时的MDD的优势比为0.88,表示患病风险很低。换句话说,如果一个通常在凌晨1点左右睡觉的人改在凌晨前睡觉,睡同样的时间,他们可以降低23%的风险;如果他们在晚上11点前睡觉,他们可以降低约40%的风险。
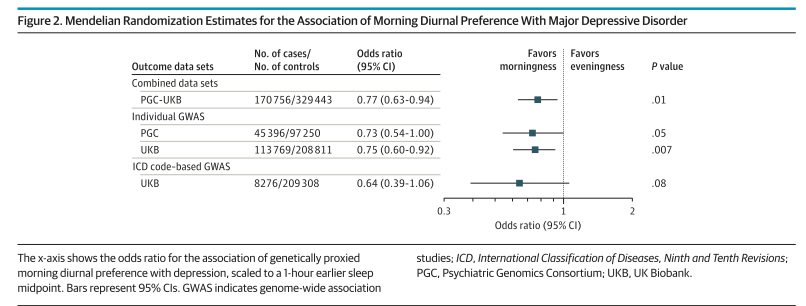
昼夜偏好与重度抑郁障碍的关系
也有证据表明,睡眠时相推迟综合症与MDD风险和抑郁症状增加有关,特别是昼夜节律紊乱的人中,这可能是一种严重的夜间偏好。睡眠时相推迟综合症是一种与生物钟有关的睡眠问题,是昼夜生物节律睡眠障碍。
研究数据与最近一项随机临床试验的结果一致,该干预试验改变了晚间昼夜偏好的人的睡眠时间。多方面的干预措施包括睡眠时间、进餐时间、光照、咖啡因摄入、午睡行为和运动行为,这一干预措施使睡眠-觉醒时间平均提前了2个小时,并促进了昏暗条件下褪黑素的出现,且干预措施没有导致睡眠剥夺或昼夜节律失调。研究结果发现:参与干预组的人员总体抑郁、焦虑和压力量表得分都有所改善,抑郁和压力亚表的得分也有所改善。
而这项试验为干预措施的可行性提供了证据,即在不缩短睡眠等情况下产生了睡眠和昼夜节律的转变。虽然这项试验也支持晨起对情绪的保护,但该研究规模较小(n = 22),而且没有硬性的临床终点。
对于那些想要将作息时间表提早的人,资深作者 Celine Vetter提供了以下建议:
她说。"早上可以喝杯咖啡。方便的话,步行或骑自行车上班,晚上将电子产品调暗。"
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑郁风险#
79
#研究发现#
67
已拜读,受益匪浅。
81
#风险降低#
59
#睡觉#
85
#哈佛#
64