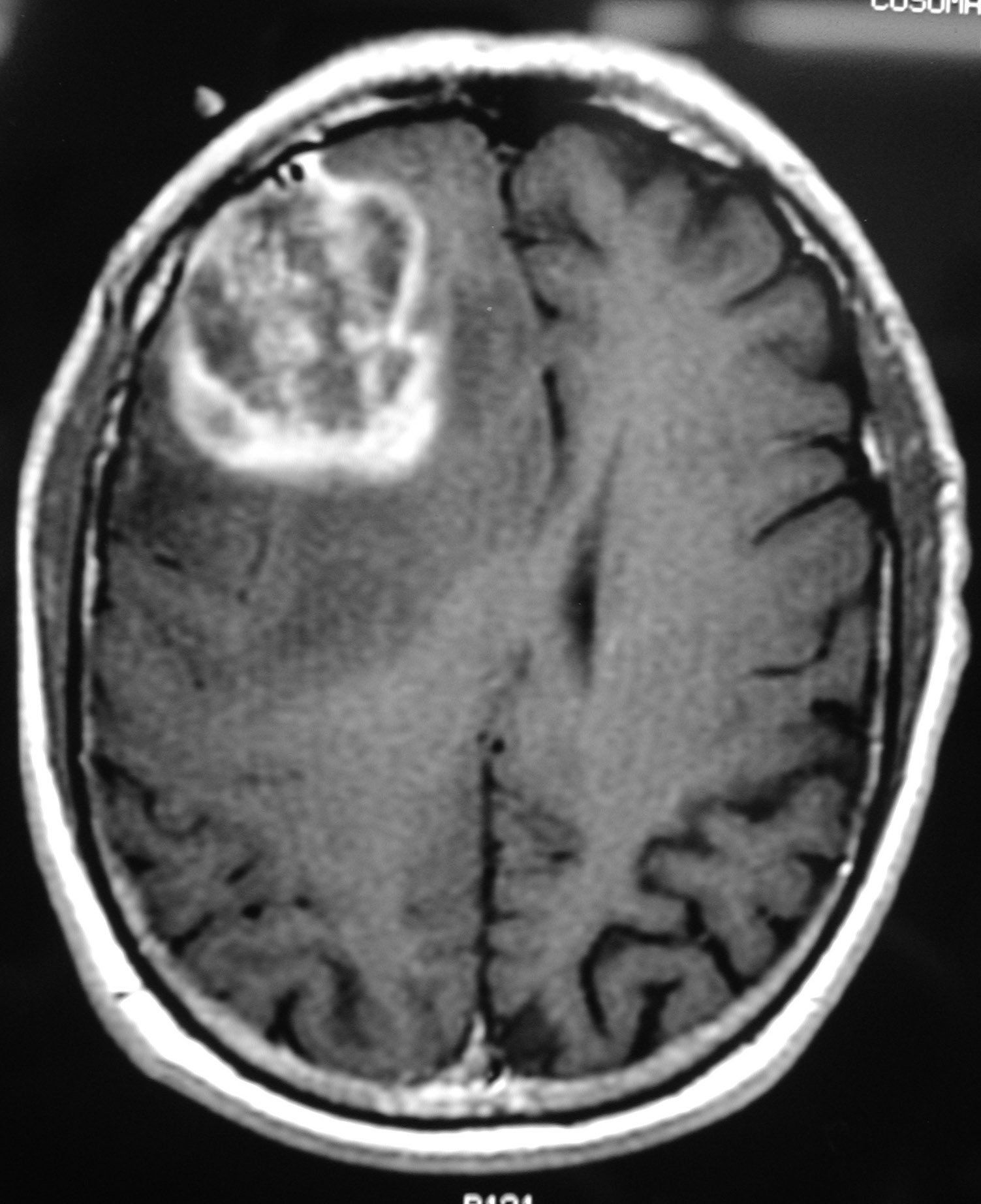
新型联合化疗方案有望显著改善胶质母细胞瘤的治疗效果
2018-01-29 MedSci MedSci原创
羟基脲是一种化疗及抗逆转录病毒药物,被用于治疗慢性粒细胞白血病、骨髓增生性疾病和镰刀型细胞贫血症等疾病。近日麻省总医院(MGH)的研究人员发现,将化疗药物羟基脲加入到目前的胶质母细胞瘤化疗方案中可显著提高模式动物的存活率。
新型联合化疗方案有望显著改善胶质母细胞瘤的治疗效果
羟基脲是一种化疗及抗逆转录病毒药物,被用于治疗慢性粒细胞白血病、骨髓增生性疾病和镰刀型细胞贫血症等疾病。近日麻省总医院(MGH)的研究人员发现,将化疗药物羟基脲加入到目前的胶质母细胞瘤化疗方案中可显著提高模式动物的存活率。
麻省总医院的Bakhos
Tannous博士说:“通过对原有药物的重新评价,我们证明了已经上市的化疗药物羟基脲与替莫唑胺对原发性和复发性胶质母细胞瘤具有显著的协同抗癌作用。这种组合在不同小鼠模型中均证明有效,模式动物的存活率显著增加,其中40-60%的模式动物的肿瘤组织消失。”
在过去的20年中,替莫唑胺(TMZ)在外科手术和放射治疗中的一直被用于胶质母细胞瘤的治疗,能够使患者的两年生存率从11%提高到27%。 但在接受这种治疗方案的患者中,仍在90%的患者在五年内死亡,主要因素来自肿瘤细胞对替莫唑胺产生的耐药性。
预计基于该项研究结果的I期临床试验即将开展,这对于胶质母细胞瘤患者无疑是令人振奋的消息。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/72049/combination-chemotherapy-glioblastoma/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胶质母细胞#
80
#治疗效果#
52
#母细胞瘤#
76
#联合化疗#
60
#细胞瘤#
64