SHPCS 2013:胰腺癌的分子标志物:整合素(Integrin)α6β4
2013-08-22 Kathleen L.O'Connor MedSci原创
第四届胰腺癌上海论坛(SHPCS)上,Kathleen L.O'Connor进行胰腺癌相关报告。侵袭和转移是导致大多数肿瘤患者治疗失败和死亡最主要原因,其过程涉及机体一系列基因结构和功能的异常,其中黏附分子起着重要的作用。整合素( integrins) 是肿瘤细胞表面的一种黏附分子,它可以介导细胞间、细胞与基质间相互作用,参与肿瘤侵袭和转移
第四届胰腺癌上海论坛(SHPCS)上,Kathleen L.O'Connor进行胰腺癌相关报告。侵袭和转移是导致大多数肿瘤患者治疗失败和死亡最主要原因,其过程涉及机体一系列基因结构和功能的异常,其中黏附分子起着重要的作用。整合素( integrins) 是肿瘤细胞表面的一种黏附分子,它可以介导细胞间、细胞与基质间相互作用,参与肿瘤侵袭和转移的过程。整合素α6β4 是整合素家族中的重要成员之一,其在肿瘤细胞中表达量的增高或减少会影响肿瘤细胞的生物学行为。
整合素α6β4在PDAC早期上调并在进程中持续高表达;
整合素α6β4协调控制了胰腺癌细胞中AREG、EREG和MMP1的表达;
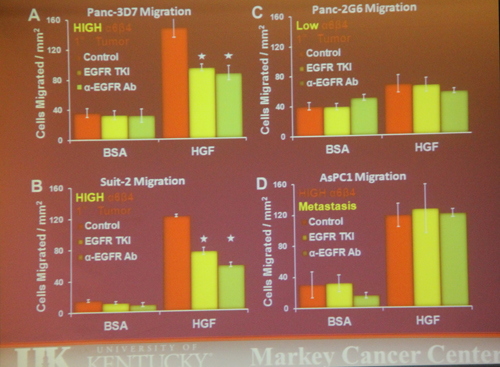
在高度α6β4表达的细胞中抑制EGFR可同时阻断HGF趋化和3D培养的入侵;
整合素α6β4和HGF信号通路刺激AREG分泌,AREG分泌可以指向前缘;
我们已经确定在EGFR和信号通路之间有一种小的物质可以管理肿瘤细胞入侵;
转移来的AsPC1细胞抑制了EGFR,因此建议通路绕行EGFR存在依赖。
肿瘤的发生和转移与整合素α6β4 的密切相关性已引起国内外学者的关注,这方面的研究成果将为探求肿瘤的发生、发展机制提供重要的新线索,是未来探 求肿瘤生长机制及制定靶点治疗手段的方向之一。深入研究整合素α6β4 通路在肿瘤的发生和转移中的作用具有重要的生物学和临床意义,相关的研究有望为肿 瘤治疗提供辅助方法和药物。
原始出处:
O'Connor KL, Chen M, Towers LN.Integrin α6β4 cooperates with LPA signaling to stimulate Rac through AKAP-Lbc-mediated RhoA activation.Am J Physiol Cell Physiol. 2012 Feb 1;302(3):C605-14.
Chen M, Sastry SK, O'Connor KL.Src kinase pathway is involved in NFAT5-mediated S100A4 induction by hyperosmotic stress in colon cancer cells.Am J Physiol Cell Physiol. 2011 May;300(5):C1155-63.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#SHPCS#
65
#PCS#
74
#integrin#
81
#标志物#
67
#整合素#
77