J Thorac Oncol:尼拉帕利一线维持治疗中国铂敏感的广泛期小细胞肺癌患者的3期临床试验结果
2021-05-01 Nebula MedSci原创
尼拉帕利作为维持疗法,适度改善了铂敏感的ES-SCLC患者的PFS
最新的流行病学分析显示,肺癌是中国年龄标准化发病率第二高(35.1例/10万人)的癌症,且死亡率最高(30.9例/10万人)。2010年-2014年的中国肺癌患者的5年存活率为19.8%。
ZL-2306-005是一项随机、双盲、多中心的3期研究,旨在评估PARP抑制剂尼拉帕利(niraparib)用作中国铂敏感的广泛期小细胞肺癌(ES-SCLC)患者一线维持治疗的有效性和安全性。
该研究将经标准化的、以铂类为基础的、一线化疗后获得完全/部分缓解(CR/PR)的患者随机分成了两组(2:1),予以尼拉帕利或安慰剂(300 mg[基线体重≥77 kg,血小板计数≥150000/μL]或200 mg),每日1次,直至病情进展或出现不可接受的毒性反应。主要终点为无进展生存期(PFS)和总生存期(OS)。次要终点包括调查员评估的PFS和安全性。
由于ES-SCLC治疗环境的改变,ZL-2306-005试验被提前终止(数据截止时间:2020年3月20日)。2018年7月至2020年2月期间,筛查的272名患者中有185名被随机分至两组(尼拉帕利组:n=125[CR=1,PR=124];安慰剂:n=60[CR=1,PR=59])。
主要终点PFS(A)和OS(B)
尼拉帕利组和安慰剂组的中位PFS分别为1.54个月(95%CI 1.41-2.69)和1.36个月(1.31-1.48;危险比[HR] 0.66[95%CI 0.46-0.95];p=0.0242),中位OS分别为9.92个月(9.33-13.54)和11.43个月(9.53-未达到;HR 1.03[95%CI 0.62-1.73];p=0.9052)。调查者评估的PFS中位数分别为1.48个月(1.41-2.56)和1.41个月(1.31-2.00;HR 0.88[95%CI 0.61-1.26];p=0.4653)。
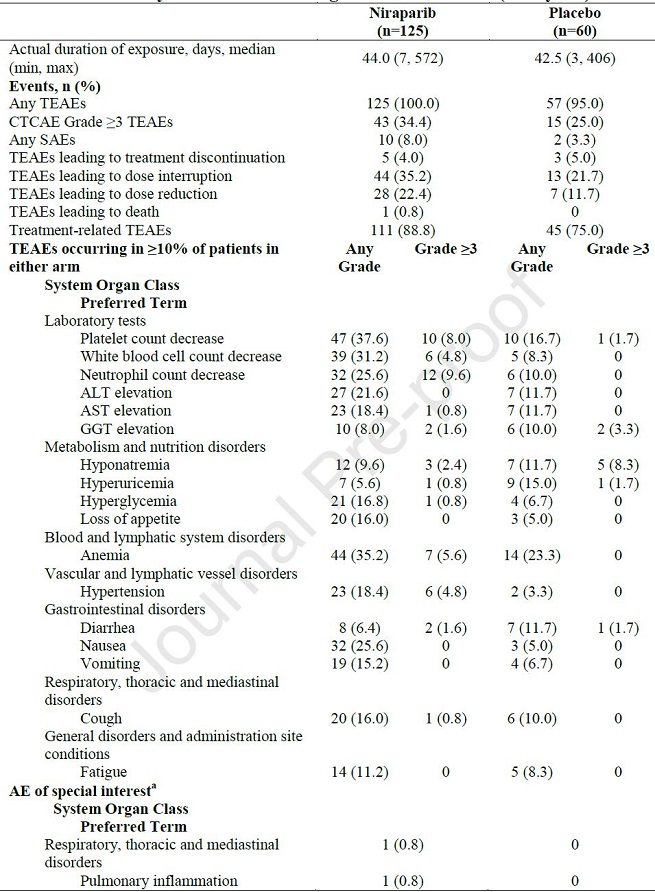
不良事件
尼拉帕利组和安慰剂组≥3级的不良事件发生率分别为34.4%和25.0%。
综上所述,ZL-2306-005未到达主要终点。然而,尼拉帕利作为维持疗法,适度改善了铂敏感的ES-SCLC患者的PFS,耐受性良好,且没有新的安全信号。
原始出处:
Ai Xinghao,Pan Yueyin,Shi Jianhua et al. Efficacy and Safety of Niraparib as Maintenance Treatment in Patients with Extensive-Stage Small Cell Lung Cancer after First-Line Chemotherapy: A Randomized, Double-Blind, Phase 3 Study. J Thorac Oncol, 2021, undefined: undefined. https://doi.org/10.1016/j.jtho.2021.04.001
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#3期临床#
67
#肺癌患者#
111
#Oncol#
73
#铂#
101
#THORAC#
77
#一线维持治疗#
114
#广泛期小细胞肺癌#
87
#3期临床试验#
80
战胜病魔
103
JTO上有很多不错的好文章,谢谢梅斯及时上新
100