Clinical Cancer Research:难治性前列腺癌耐药新靶点浮出水面
2020-08-08 Muse Fan MedSci原创
染色体17q22区域基因拷贝数的缺失与mCRPC患者恩杂鲁胺的耐药发生相关,并且17q22基因拷贝数缺失的mCRPC患者总生存率更低,这为未来寻找耐药治疗靶点提供了依据。
去势抵抗性前列腺癌(Castration Resistant Prostate Cancer, CRPC)是指前列腺癌患者经过手术或药物去势后仍然出现PSA升高和影像学进展,而mCRPC(Metastatic CRPC)是指出现远处转移的CRPC患者。mCRPC是前列腺癌治疗的难点,也是前列腺癌致死的最主要原因。雄激素受体拮抗剂恩杂鲁胺是治疗mCRPC患者的主要药物之一,该药物在临床试验中已被证实可以提高mCRPC患者的生存率。然而肿瘤仍然会发生进展,部分患者会出现恩杂鲁胺耐药性,此时临床治疗方法的选择非常有限。目前对恩杂鲁胺耐药的机制尚不清楚,因此探索耐药的发生机制对于延缓mCRPC的进展和寻找治疗靶点都具有重要的意义。
doi:10.1158/1078-0432.CCR-19-2303
近日,发表在Clinical Cancer Research的一篇研究对恩杂鲁胺耐药和未使用恩杂鲁胺治疗的mCRPC患者基因组特征进行了比较,发现耐药患者特定染色体区域基因拷贝数的缺失与耐药和预后不良相关。
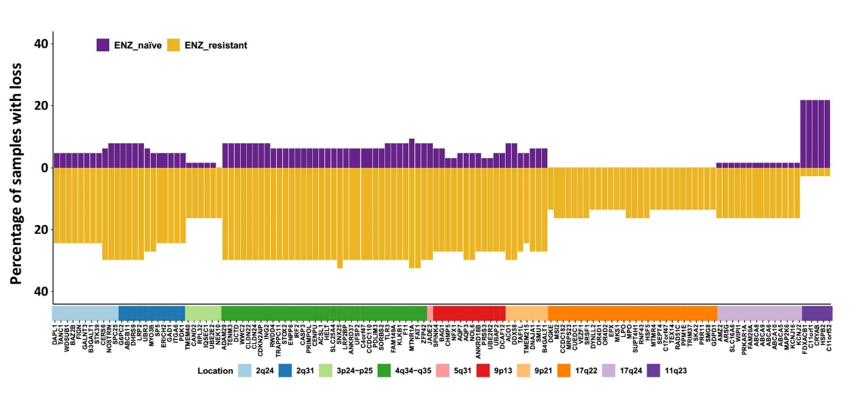
图1. 两组患者各染色体区域基因拷贝数丢失病例占比
该研究对64例未接受恩杂鲁胺治疗和37例恩杂鲁胺耐药的mCRPC患者的组织活检标本进行了全基因组测序。首先通过对比基因拷贝数发现,两组标本在10个染色体区域存在基因拷贝数差异,恩杂鲁胺耐药患者在其中9个区域基因拷贝数都低于未接受恩杂鲁胺治疗患者,耐药患者基因拷贝数丢失显著高于未接受治疗患者(图1)。
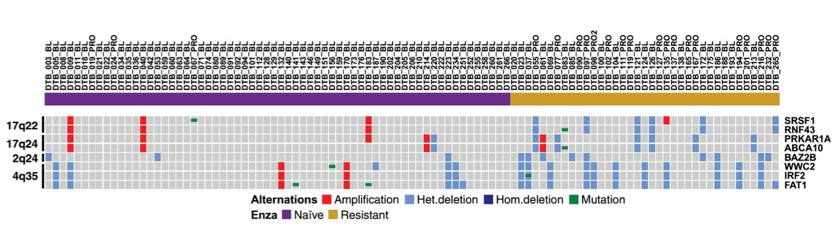
图2.两组患者抑癌基因差异表达情况
这9个染色体区域包含了124个蛋白编码基因,通过与先前文献报道的对比,研究者发现其中8个基因为肿瘤抑制基因。进一步的分析发现位于8个基因中位于17q22区域的RNF43和SRSF1基因的缺失只在恩杂鲁胺耐药的患者中出现(6/37)(图2),生存分析的结果表明17q22缺失的患者中位总生存期(8.9月)显著低于未缺失的患者(19.3月)(图3)。
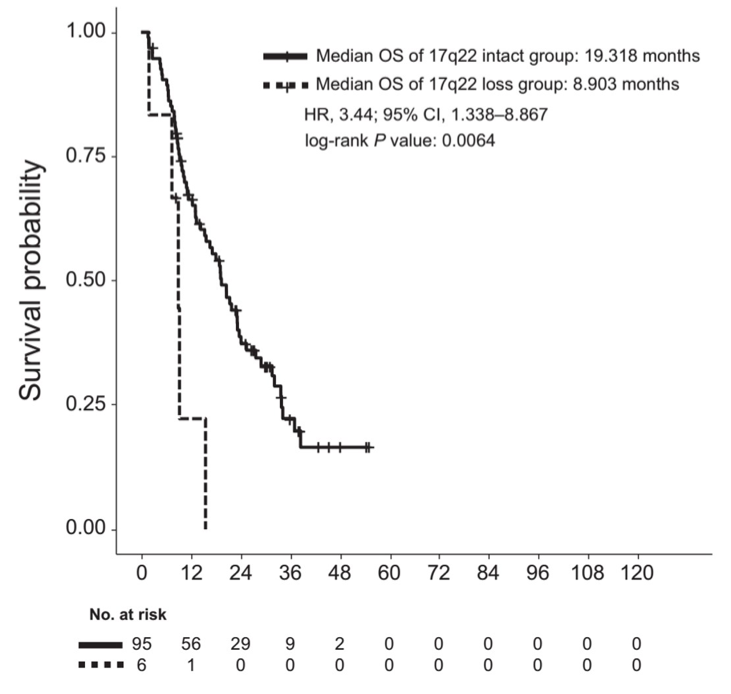
图3. 17q22缺失组与对照组生存分析
该研究得出:染色体17q22区域基因拷贝数的缺失与mCRPC患者恩杂鲁胺的耐药发生相关,并且17q22基因拷贝数缺失的mCRPC患者总生存率更低,这为未来寻找耐药治疗靶点提供了依据。
原始出处:Guan X, Sun D, Lu E, Urrutia JA, Reiter RE, Rettig M, et al. Copy Number Loss of 17q22 Is Associated with Enzalutamide Resistance and Poor Prognosis in Metastatic Castration-Resistant Prostate Cancer. Clinical Cancer Research 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新靶点#
95
#clinical#
68
#难治性#
82
#Research#
68
前列腺癌相关研究,学习了,谢谢梅斯
108