JAHA:脑出血3个月后不受控高血压对患者预后的影响
2021-05-18 MedSci原创 MedSci原创
在ICH幸存者中,60%以上的患者3个月时伴有未受控的高血压,其中大多数病例为降压治疗不充分。三个月时的血压测量结果与较高的卒中复发风险和死亡率相关。
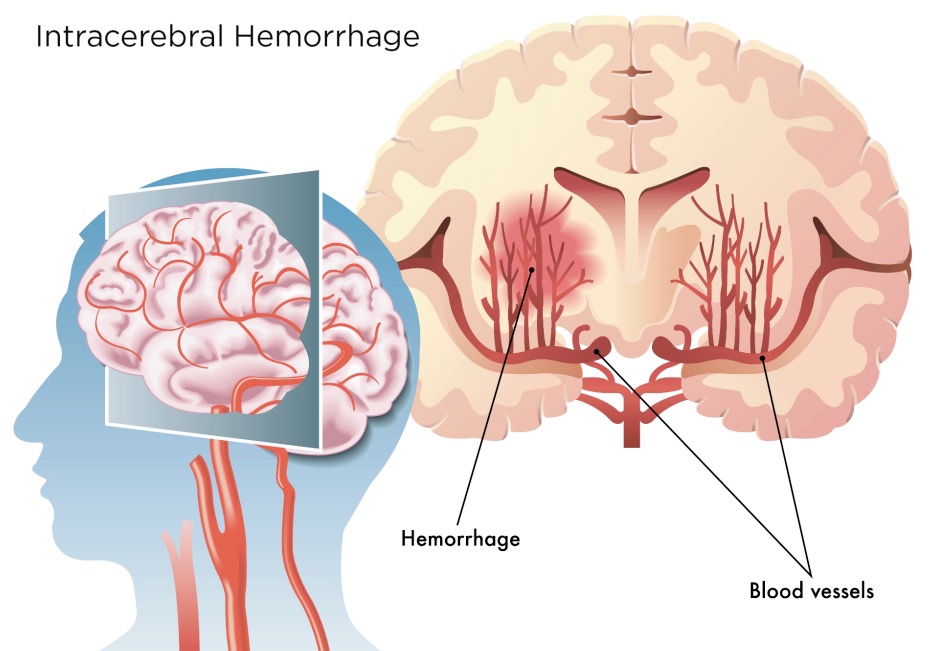
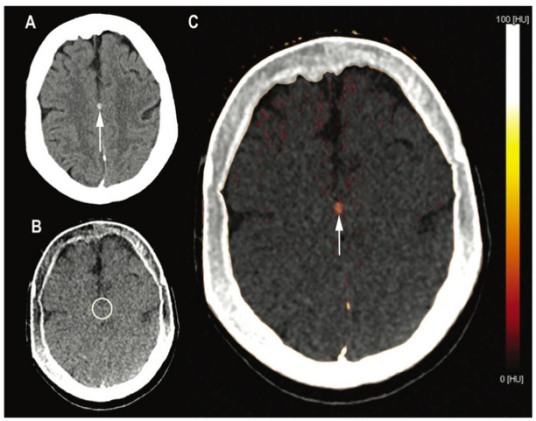
脑出血(ICH)幸存者具有较高的卒中复发风险,这与血压控制有关。由于大多数复发性卒中事件发生在ICH发生后的12至18个月内,因此快速控制血压可能至关重要。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员分析了麻省总医院(n=1305)和香港大学(n=523)的数据,并将ICH后3个月内的高血压归类为控制、治疗不足或对治疗有抵抗,并明确以下内容:(1)高血压不受控制的危险因素;(2)控制3个月的高血压是否与卒中复发和死亡率相关。

研究随访了1828名ICH幸存者,中位时间为46.2个月。ICH发生后头3个月,234例患者中仅有9例(4%)患者出现复发性卒中。
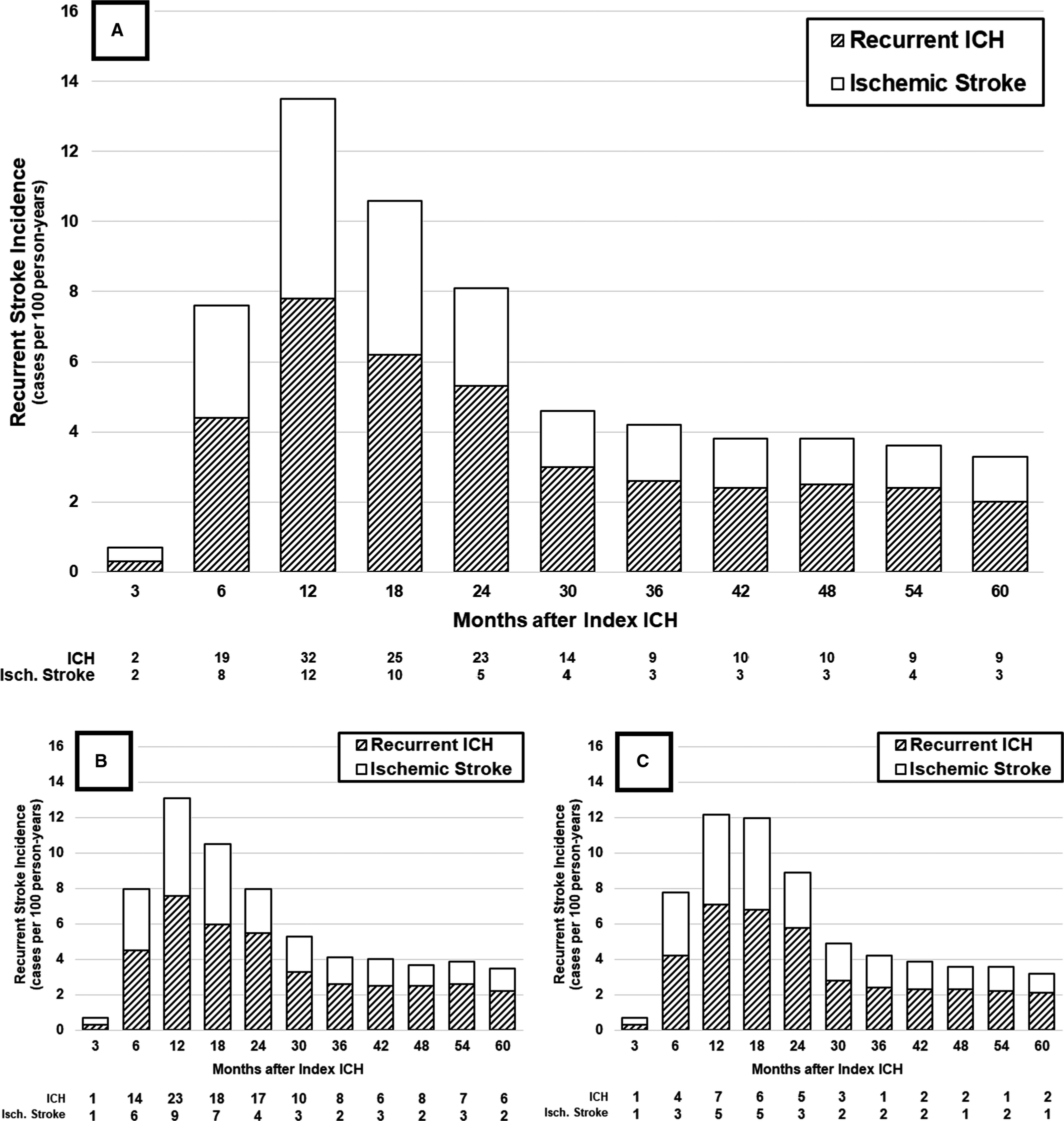
ICH后复发性卒中风险
在3个月时,713名(39%)参与者高血压得到了控制,其中755名(41%)患者降压治疗治疗不充分,而360名(20%)患者出现治疗抵抗性高血压。黑人、西班牙裔和亚洲人以及ICH时血压升高会增加3个月时高血压不受控制的风险(所有P<0.05)。在长期随访中,3个月未控制的高血压与卒中复发和死亡率相关(所有P<0.05)。
由此可见,在ICH幸存者中,60%以上的患者3个月时伴有未受控的高血压,其中大多数病例为降压治疗不充分。三个月时的血压测量结果与较高的卒中复发风险和死亡率相关。黑人、西班牙裔和亚洲裔ICH幸存者以及伴有严重急性高血压反应的患者出现不受控高血压的风险最高。
原始出处:
Alessandro Biffi.et al.Impact of Uncontrolled Hypertension at 3 Months After Intracerebral Hemorrhage.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.020392
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#患者预后#
81
#AHA#
77
讲得真好
0
强
107
学到了#高血压#
123