SCI REP:疑似深静脉血栓形成的患者年龄相关的D-二聚体检测的诊断价值如何?
2017-07-04 xing.T MedSci原创
总之,这些数据概述了在疑似DVT的年轻患者中D-二聚体测试的临床相关限制,其表明设置年龄适应性临界值的必要性。需要进一步的研究来解释炎症在静脉血栓形成的病理生理学和诊断中的作用。
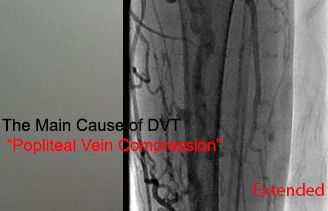
既往的研究已经调查了年龄对疑似深静脉血栓形成(DVT)的老年患者D-二聚体检测的影响,但是涉及广泛年龄范围的样本中D-二聚体年龄相关的诊断价值的数据十分有限。
近日,Scientific reports 杂志上发表了一篇研究文章,该研究是在来自于VTEval项目(NCT02156401)的500例疑似DVT患者中进行,旨在确定D-二聚体年龄特异性的诊断准确性,并将其与C反应蛋白(CRP)(炎症标志物)进行比较。
研究人员发现与≥60岁的患者相比,60岁以下患者D-二聚体的敏感性较低(Δ为-16.8%),而特异性要高出27.9%。在女性、无诱因的DVT、低血栓负荷和远端DVT的患者中,其敏感度水平最低。将D-二聚体阈值固定在0.25mg/L,FEU导致60岁以下患者敏感性升高,对于近端DVT的患者假阴性减少了40.0%,对于远端DVT患者减少了50.0%。在60岁以下的患者中,D-二聚体和CRP在近端和远端DVT中表现出了相似的诊断性能(p> 0.05)。
原始出处:
Jürgen H. Prochaska,et al. Age-related diagnostic value of D-dimer testing and the role of inflammation in patients with suspected deep vein thrombosis.Scientific reports. 2017. https://www.nature.com/articles/s41598-017-04843-x
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
68
#静脉血#
64
#诊断价值#
62
#二聚体#
60
学习了学习了学习了学习了
101
#年龄相关#
66
#体检#
56
#D-二聚体#
70
#静脉血栓形成#
60