Circulation:无接触技术可显著降低冠脉搭桥术后移植静脉的闭塞率
2021-10-12 Nebula MedSci原创
对于进行冠状动脉旁路移植术的患者,与传统的静脉采集方法相比,无接触技术显著降低了移植术后移植静脉闭塞的风险,改善了患者的预后
移植静脉阻塞被认为是冠状动脉旁路移植术的主要挑战。既往研究表明,与传统方法相比,静脉移植物采集的非接触技术可以降低闭塞率。但是,关于非接触技术的临床效益和普遍性的证据仍比较匮乏。
从2017年4月至2019年6月期间,来自7家医院接受冠状动脉旁路移植的2655位患者被随机(1:1)分成两组,接受无接触技术或传统方法进行静脉采集。主要终点是第3个月时的CT检查发现的移植静脉阻塞率。次要终点包括12个月移植静脉阻塞率、心绞痛复发和主要不良心脑血管事件。
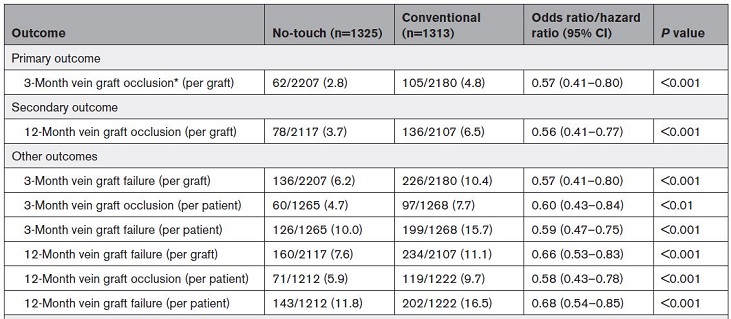
两组的各种预后
在随访过程中,2533位(96.0%)受试患者在冠状动脉旁路移植术后3个月时进行了CT血管造影检查,2434位(92.2%)在术后12个月时进行了CT血管造影检查。无论是在3个月时还是12个月时,无接触组的移植静脉阻塞率都显著低于传统方法组(3个月:2.8% vs 4.8%,优势比[OR] 0.57, 95% CI 0.41-0.80, p<0.001;12个月:3.7% vs 6.5%,OR 0.56, 95% CI 0.41-0.76; p<0.001)。
此外,12个月时,非接触组患者的心绞痛复发率也较低(2.3% vs 4.1%;OR 0.55, 95% CI 0.35-0.85, p<0.01)。两组主要不良心脑血管事件发生率无显著差异。随访3个月时,无接触技术与较高的腿部伤口手术干预率相关(10.3% vs 4.3%,OR 2.55, 95% CI 1.85-3.52, p<0.001)。
综上所述,对于进行冠状动脉旁路移植术的患者,与传统的静脉采集方法相比,无接触技术显著降低了移植术后移植静脉闭塞的风险,改善了患者的预后。
原始出处:
Meice Tian, et al. No-Touch Versus Conventional Vein Harvesting Techniques at 12 Months After Coronary Artery Bypass Grafting Surgery: Multicenter Randomized, Controlled Trial. Circulation. 2021;144:1120–1129
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#冠脉搭桥术#
58
#静脉#
56
#搭桥#
97
#搭桥术#
67
#冠脉搭桥#
86
8起?。!咯武器咳咳卡塔U盾TM投
79