Lancet Oncol:TERT启动子UTSS区域高度甲基化是儿童脑肿瘤进展的预测标记
2013-08-27 echo1166 dxy
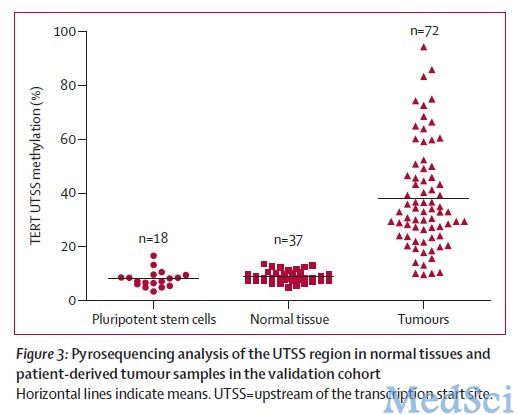
研究要点:TERT启动子甲基化可作为儿童恶性脑肿瘤的生物标记和预后判断标记。在儿童恶性脑肿瘤中,当肿瘤从低级别向高级别转化时,UTSS甲基化增加。TERT启动子UTSS区域的高度甲基化与肿瘤中TERT的表达相关。在儿科神经系统肿瘤领域中,鉴定得到对恶性疾病有提示意义的生物标记是十分重要的方面。这有助于建立评估疾病出现进展的方法。加拿大多伦多大学的Pedro Castelo-Branco等为了探
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肿瘤进展#
34
#Lancet#
35
#启动子#
43
#预测标记#
40
#Oncol#
31
#脑肿瘤#
28