

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

2018-04-10 杨中华 脑血管病及重症文献导读
60岁,男性。表现为眩晕,勾引障碍和左侧无力。



作者 杨中华 首都医科大学附属北京天坛医院 大面积梗死的患者经过再灌注治疗往往预后不良,甚至再灌注性水肿或出血。ASPECTS评分是一项10分评分系统,评价平扫脑CT预先设定前循环区域的脑实质低密度作为早期缺血性特征。在几项大型急性缺血性卒中血管内治疗的随机临床试验中,采用这项评分标准作为影像学纳入标准。ASPECTS评分能够识别哪些急性缺血性卒中能够从再灌注治疗中获益,或有害。
卒中的临床前模型表明,静脉使用格列本脲可减轻脑水肿、改善生存率。我们对大面积半球梗死患者进行了研究,旨在评估静脉使用格列本脲能否安全的减轻脑水肿、降低去骨瓣减压的需要、改善患者的临床结果。 在这项双盲、随机、安慰剂对照的2期临床试验中,我们纳入了诊断前循环大面积半球梗死10小时内的患者(18-80岁),基线弥散加权MRI图像显示病变体积82–300 cm3。将患者按1:1随机分为安慰剂组或静
研究者使用使用酒精销售法的差异进行了一项观察性队列研究,探究酒精摄入量与心脏病的关系,并作为一种自然实验。该研究纳入了2005-2010年间≥21岁的1106968名住院患者,根据所在区域酒精的限制情况分为“湿”县(没有酒精的限制)和“干”县(酒精销售全面禁止)。酒精滥用和酒精性肝病的流行率发生率数据用于验证分析。研究的主要心血管终点为房颤、急性心肌梗死和充血性心力衰竭。数据显示,湿县居民酒精滥用
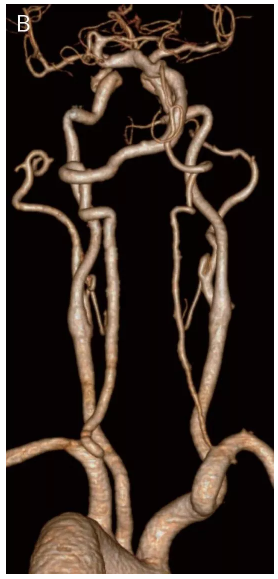
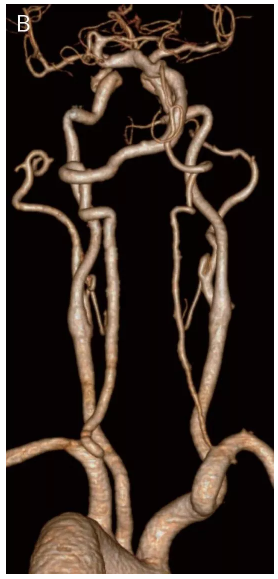
61岁男性,因“言语不清伴左侧肢体无力20余天”入院。患者表现为耳聋、言语不清、眩晕不敢睁眼。既往有高血压、糖尿病、心房颤动病史及大量吸烟、饮酒病史。
对于冠心病或脑梗死患者,他汀是最基本治疗药物之一,只要没有禁忌证,所有患者均应长期服用。我们知道,发生冠心病(包括心肌梗死)和脑梗死的根本原因是动脉粥样斑块形成,而胆固醇是形成动脉粥样斑块的主要原料,没有胆固醇就没有动脉粥样硬化斑块,也就不会有心肌梗死和脑梗死。
内囊是大脑皮层与脑干、脊髓联系的神经纤维通过的一个部位的名称,位于基底神经节与丘脑之间。通往大脑皮层的运动神经纤维和感觉神经纤维,均经内囊向上呈扇形放射状分布。肌紧张和肌肉运动是由脑干网状结构控制的。脑桥网状核是网状结构易化区域之一。脑桥的被盖和延髓网状结构背外侧部、中脑中央灰质以及下丘脑后部和丘脑中缝核群等共同对同侧伸肌起调节作用,主要是易化性影响。另外,在大脑-脑桥-小脑之间形成一个环形联系,


梅斯医学MedSci APP
医路相伴,成就大医
#蛛网膜#
0
#Neurol#
0
#继发#
80
学习了受益匪浅
104
学习了.
80
学习了
88
学习一下谢谢
97
非常好.谢谢分享
87
学习学习学习
75