BMJ:PD-L1表达阴性患者 PD-1/PD-1抑制剂也能大幅延长生存期
2018-11-09 贾朝娟 环球医学
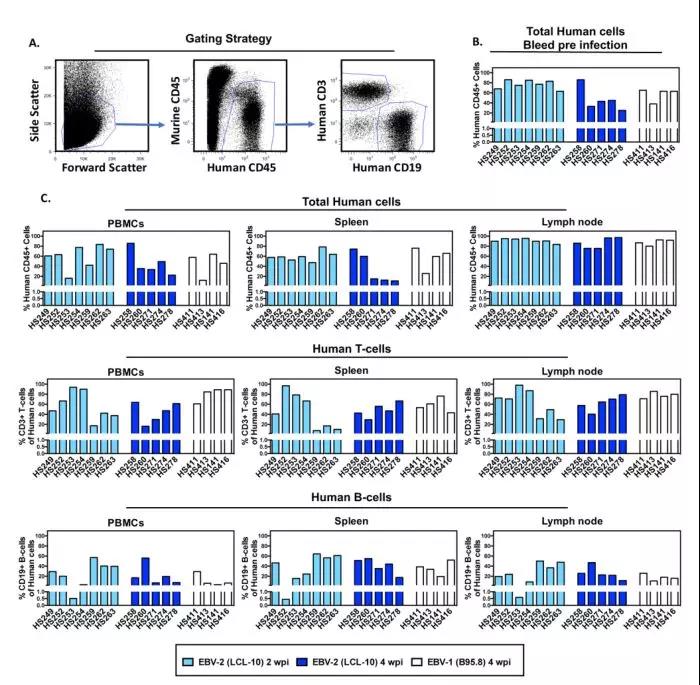
免疫抑制和逃逸是恶性肿瘤细胞的特征之一。程序性细胞死亡1(PD-1)和程序性细胞死亡配体1(PD-L1)轴,不仅在生理免疫平衡中起着关键作用,而且是癌细胞免疫逃逸的一种手段,因此成为有价值的治疗靶点。以PD-1和PD-L1为靶点的抗体的开发和应用,将癌症治疗推入了新纪元。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMJ#
73
#抑制剂#
70
#PD-L1表达#
0
#PD-L1#
77
#PD-1抑制剂#
80
#生存期#
69
温故而知新
101
国内用的还是太少
93