AJKD:卡格列净的“急性肾损伤”警告标签也许并没有想象中的那么可怕!
2022-02-11 MedSci原创 MedSci原创
钠/葡萄糖共转运蛋白2 (SGLT2)抑制剂是一种相对较新的口服降糖药物,在大型心血管安全试验中已被证明可以降低主要心血管和心力衰竭的风险。
钠/葡萄糖共转运蛋白2 (SGLT2)抑制剂是一种相对较新的口服降糖药物,在大型心血管安全试验中已被证明可以降低主要心血管和心力衰竭的风险。这些试验还表明,SGLT2抑制剂可以延缓肾小球滤过率(eGFR)随时间下降的进程。尽管SGLT2抑制剂的心血管安全性已被证实,但其导致肾功能急性下降的风险仍存在争议。
SGLT2抑制剂的标签中明确包括关于急性肾损伤(AKI)风险增加的警告。这些警告来自于上市后的监测数据,这些数据表明2型糖尿病(T2DM)和肾功能正常的患者发生AKI的风险增加。此前,在一项名为“卡格列净与糖尿病肾病肾脏事件的临床评估(CREDENCE)”试验发现,卡格列净可降低2型糖尿病(T2DM)和慢性肾脏疾病(CKD)患者肾功能衰竭的风险和相关结局。这项对CREDENCE试验数据的分析研究了卡格列净对肾脏相关不良事件(AEs)发生率的影响。
本研究为一项随机,双盲,安慰剂对照,多中心国际试验,纳入4401名T2DM、CKD和尿白蛋白-肌酐比值>300- 5000 mg/g的试验参与者吗,参与者被随机分配到卡格列净100 mg/d或安慰剂组。
分析结果显示,卡格列净与肾脏相关不良事件的总发生率降低相关,严重肾相关不良事件和急性肾损伤结果一致。在3个eGFR层中,卡格列净组与安慰剂组相比,肾相关不良事件的发生率较低,AKI组的结果相似。与安慰剂相比,卡格列净组在AKI事件发生后30天内肾功能完全恢复的频率更高(53.1%对35.4%;优势比为2.2[95%CI,1.0-4.7];P=0.04)。
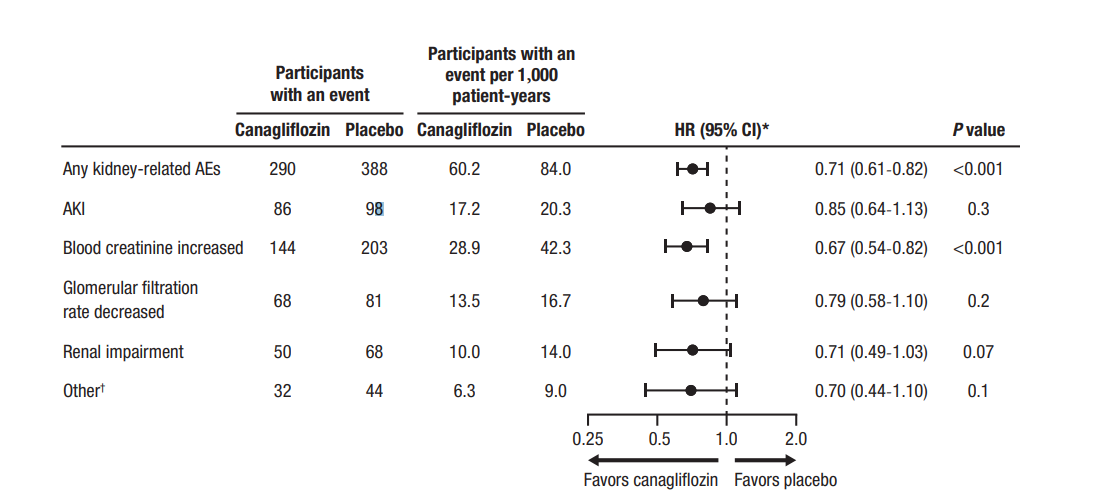
与安慰剂相比,卡格列净对肾脏相关不良事件(AEs)风险的影响
综上所述,本研究显示,与安慰剂治疗相比,在T2DM和CKD患者中,canagliflozin与较低的严重和非严重肾脏相关AEs(包括AKI)发生率相关。这些数据强调了卡纳格列净在这一人群中的安全性。
参考文献:Hiddo J.L. Heerspink, Megumi Oshima, Hong Zhang, et al,Canagliflozin and Kidney-Related Adverse Events in Type 2 Diabetes and CKD: Findings From the Randomized CREDENCE Trial, American Journal of Kidney Diseases, Volume 79, Issue 2, 2022, Pages 244-256.e1, ISSN 0272-6386, https://doi.org/10.1053/j.ajkd.2021.05.005.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很好
131
学无止境
0
#损伤#
102
好文章,学习到了,谢谢。
129