Ⅳ期结直肠癌原发肿瘤切除术或过度使用
2015-01-28 cmt 中国医学论坛报
美国M.D.安德森癌症研究中心的一项回顾性队列研究表明,尽管大多数Ⅳ期结直肠癌">结直肠癌患者均接受原发肿瘤切除术,但从2001年开始,原发肿瘤切除手术呈现逐渐递减趋势。虽然原发肿瘤切除比率下降了,但患者存活却较以往有所改善,提示原发肿瘤切除术对于患Ⅳ期结直肠癌患者的治疗可能不是常规必要的。论文1月14日在线发表于《美国医学会 外科学》(JAMA Surg)杂志。 该研究旨在评估原发肿瘤切
美国M.D.安德森癌症研究中心的一项回顾性队列研究表明,尽管大多数Ⅳ期结直肠癌">结直肠癌患者均接受原发肿瘤切除术,但从2001年开始,原发肿瘤切除手术呈现逐渐递减趋势。虽然原发肿瘤切除比率下降了,但患者存活却较以往有所改善,提示原发肿瘤切除术对于患Ⅳ期结直肠癌患者的治疗可能不是常规必要的。论文1月14日在线发表于《美国医学会 外科学》(JAMA Surg)杂志。
该研究旨在评估原发肿瘤切除术在美国Ⅳ期结直肠癌患者中的使用情况。通过对美国国立癌症研究所调查、流行病学和结直肠癌登记最终结果的数据进行分析,在1998年1月1日至2010年12月30日诊断为Ⅳ期结的直肠癌患者中,比较了接受和未接受原位肿瘤切除患者之间的人口统计学和临床因素。
在纳入的64157例Ⅳ期结肠癌患者中,有43 273 例(67.4%)患者接受原位肿瘤切除术。每年行原发肿瘤切除术的比率从1988年的74.5%降至2010年的57.4%(P<0.001),并且1998~2001年与2001~2010年的年度变化最为明显(-0.41%对-2.39%,P<0.001)。
与原发肿瘤切除术相关的因素为年龄(<50岁)、性别(女性)、婚姻状况(已婚)、肿瘤分级(更高分级)和有无肿瘤(有)。
中位相对存活率从1988年的8.6%增加至2009年的17.8%(P<0.001);1988 ~2001年及1996~2005年的年均变化率分别为2.18%和5.43%.
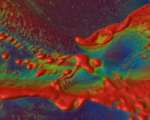
图Ⅳ期结直肠癌患者原发肿瘤切除率和患者中位相对生存率
表3. 接受原发肿瘤切除术患者的多变量分析结果
研究者指出,“目前推荐的Ⅳ期结直肠癌治疗方法为系统治疗。系统化疗和生物学治疗能控制症状,延长寿命,将不可手术的疾病转变为可手术的疾病。由于化疗和生物药物的发展,医生有了更好的系统治疗选择。几项试验证实,Ⅳ期结直肠癌患者接受伊立替康、奥沙利铂、贝伐珠单抗或帕尼单抗单独治疗或与(5-氟尿嘧啶+亚叶酸)/卡培他滨联合用药可以改善患者生存情况。 化疗方法治疗结直肠癌可以使患者受益已被证实,我们在研究中却发现2010年超过50%的患者仍然选择原发肿瘤切除术,说明目前仍存在原位肿瘤切除术的过度使用现象,建议在以后的工作中应该加强对该手术的临床决策和治疗预后的理解”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
52
#肿瘤切除#
53
#原发肿瘤#
54
不过这是回顾性研究
130
#结直肠#
48
从2001年开始,原发肿瘤切除手术呈现逐渐递减趋势。虽然原发肿瘤切除比率下降了,但患者存活却较以往有所改善,提示原发肿瘤切除术对于患Ⅳ期结直肠癌患者的治疗可能不是常规必要的。
91
很有意思
155