Immunology:热应激肿瘤细胞来源的外泌体可将Treg转化成Th17细胞从而发挥抗肿瘤作用
2017-12-09 MedSci MedSci原创
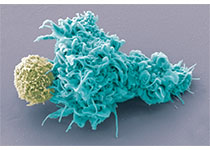
含有丰富的热休克蛋白(HSP)70的热应激肿瘤细胞(HS-TEX)来源的外泌体可显著诱导机体的抗肿瘤免疫反应。HSP70诱导的白细胞介素-6(IL-6)促进IL-17的表达并引起前列腺肿瘤的排斥反应。然而,HS-TEXs是否可将调节性T细胞(Tregs)转化为Th17细胞而表现出抗肿瘤作用则尚不清楚。在这项研究中,我们发现,与TEXs相比,HS-TEXs能更有效地刺激树突状细胞分泌IL-6。在体外
含有丰富的热休克蛋白(HSP)70的热应激肿瘤细胞(HS-TEX)来源的外泌体可显著诱导机体的抗肿瘤免疫反应。HSP70诱导的白细胞介素-6(IL-6)促进IL-17的表达并引起前列腺肿瘤的排斥反应。然而,HS-TEXs是否可将调节性T细胞(Tregs)转化为Th17细胞而表现出抗肿瘤作用则尚不清楚。
在这项研究中,我们发现,与TEXs相比,HS-TEXs能更有效地刺激树突状细胞分泌IL-6。在体外,IL-6阻断肿瘤细胞来源的转化生长因子β1诱导的Treg分化并促进Th17细胞分化。 HS-TEXs具有很强的抗肿瘤作用,能将Tregs高效转化为Th17细胞,而这一过程完全依赖于IL-6。IL-17的中和完全消除了TEXs的抗肿瘤作用,但仅部分抑制了HS-TEXs的作用。此外,我们发现高温治疗的肿瘤患者血清中IL-6和IL-17的水平升高,外周血单个核细胞中Th17细胞增加,Tregs降低。
因此,我们的研究结果表明,HS-TEX可通过IL-6将免疫抑制性Treg转化成Th17细胞,从而发挥有效的抗肿瘤作用。
原始出处:
Guo D, Chen Y, et al., Exosomes from heat-stressed tumor cells inhibit tumor growth by converting regulatory T cells to Th17 cells via IL-6. Immunology. 2017 Dec 2. doi: 10.1111/imm.12874.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肿瘤细胞#
34
#Th17#
66
#应激#
33
#Treg#
42