腰椎间盘突出,这3个问题你要懂
2016-04-18 佚名 睿医
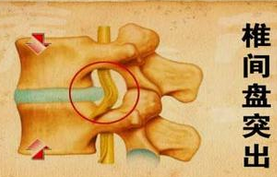
谁没有腰酸腿痛?久坐或劳累导致腰椎间盘突出,休养一段时间疼痛大多会得到改善。如果卧床休息、正规保守治疗3周以上仍无法缓解疼痛,应该及时就医。骨科专家指出,在手术治疗方法上应因人而异,采取个体化的治疗方案,可以采用微创的,尽量采用微创治疗,必须开放手术治疗的,就不应刻意追求微创。 问题1腰痛何时该看医生? 来自广西的患者陈先生,患腰椎间盘突出症有10余年时间了,每
谁没有腰酸腿痛?久坐或劳累导致腰椎间盘突出,休养一段时间疼痛大多会得到改善。如果卧床休息、正规保守治疗3周以上仍无法缓解疼痛,应该及时就医。骨科专家指出,在手术治疗方法上应因人而异,采取个体化的治疗方案,可以采用微创的,尽量采用微创治疗,必须开放手术治疗的,就不应刻意追求微创。
问题1腰痛何时该看医生?
来自广西的患者陈先生,患腰椎间盘突出症有10余年时间了,每一次发作,采用牵引、按摩、吃中药、贴药膏等保守治疗后,疼痛都会有所缓解。但从今年1月份开始腰腿痛突然加剧,各种保守治疗方法都做了,疼痛不但没有缓解,还发展到无法直立走路,晚上也睡不着觉。被折磨了几个月后,陈先生才入院治疗。
暨南大学附属第一医院骨科主任医师林宏生指出,在腰椎间盘突出症初期,主要的治疗方法是自我保护,包括理疗、卧床休息、佩戴腰围、降低工作劳动强度、减少家务劳动等,这些措施对于缓解腰腿痛有帮助。许多患者经过一段时间的保守治疗,症状会有所缓解。
但是,疾病进展了,疼痛不能缓解了,有的患者腰痛非常严重,甚至放射到小腿和足部,经过卧床休息、正规保守治疗3周以上仍无法缓解,就不要再害怕手术或者一味寻求偏方,而应该到医院进一步检查治疗。
问题2我一定要手术吗?
腰椎间盘突出该如何治疗呢?林宏生说,常见的治疗方法包括保守治疗、微创手术治疗和开放手术治疗。由于每个患者的病情严重程度、体质、合并的内科疾病等不同,所采用的治疗方法也各不相同,绝不是千篇一律。
在暨南大学附属第一医院,上述患者陈先生经核磁共振检查发现L3/4、L4/5、L5/S1椎间盘已严重退变并突出压迫神经根,杜冷丁也无法很好止痛,这种情况必须进行手术治疗。而且他的腰部由于长时间敷中药导致皮肤溃烂,强行做开放减压手术非常容易导致感染而使得手术失败,所以只能选择先做微创手术,等腰部皮肤愈合后再做开放手术。
因此,每个患者的情况不同,选择的治疗方案也应不同。林宏生说,如果腰椎间盘突出引起的腰腿痛症状不严重,短时间保守治疗后症状有改善,可以继续保守治疗;对于那些保守治疗无效,出现下肢麻木、肌肉无力者建议尽早考虑手术。因为,这些症状说明神经正在发生较难逆转的损伤,如果不尽早解除压迫,即便以后选择手术,上述症状也很难恢复。同样,如果腰腿痛反复发作十分频繁,每次犯病延续的时间很长,专家也会建议病人手术治疗。
问题3微创比传统手术更好吗?
在临床上,医生还发现腰椎间盘突出的患者常常咨询,能不能选择做微创?觉得微创手术比传统手术更好。最近,林宏生就给一名来自广州本地的71岁梁先生做了腰椎间盘微创手术。梁先生入院前1周腰腿痛的症状严重,并出现了右下肢麻木无法行走,夜晚不能平卧。
影像学检查发现,梁先生L3/4髓核脱出于右侧椎间孔,压迫相应节段的神经根。林宏生为其做了经皮侧路镜下L3/4椎间盘髓核摘除的微创手术,整个手术过程基本没有出血,手术切口只有0.8cm。术后当天梁先生的腰腿麻痛症状消失了,能自如地平卧了,术后第1天就能下地行走。
林宏生说,相比于传统的开放手术,微创手术有不少优点,比如切口小、出血少、对椎旁肌肉的损伤小、出院时间短等。
但他指出,微创手术本身也存在一定的缺陷:(1)微创并不意味着手术危险变小了,实际上微创手术的风险与开放手术相当;(2)适应症选择不恰当,微创容易出现减压不彻底,术后残留部分症状;(3)没有完全摘除椎间盘,存在复发可能;(4)微创虽然对脊柱稳定性没有太大的干扰,但是对脊柱的稳定性也没有加强作用。
所以,专家认为,对椎间盘突出症的患者来说,可以采用微创的,尽量采用微创治疗;必须开放手术治疗的,就不应勉强采用微创,手术适应症的正确选择是关键。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎间盘突出#
182
好文,值得学习,赞!
92
微创损伤较小,到对技术跟器械的要求也更高。
195
#腰椎#
95
#腰椎间盘#
104
写的比较中肯
158
算是复习了
210
腰椎间盘突出症,临床常见
154