Nat Med:局灶性癫痫的新型基因疗法
2019-01-30 佚名 生物通
英国伦敦大学学院神经学研究所的Andreas Lieb及其同事尝试在大鼠身上使用病毒介导的基因疗法,以检测它是否能减少癫痫发作以及耐受性如何。这项研究成果发表在著名期刊《Nature Medicine》上。
英国伦敦大学学院神经学研究所的Andreas Lieb及其同事尝试在大鼠身上使用病毒介导的基因疗法,以检测它是否能减少癫痫发作以及耐受性如何。这项研究成果发表在著名期刊《Nature Medicine》上。
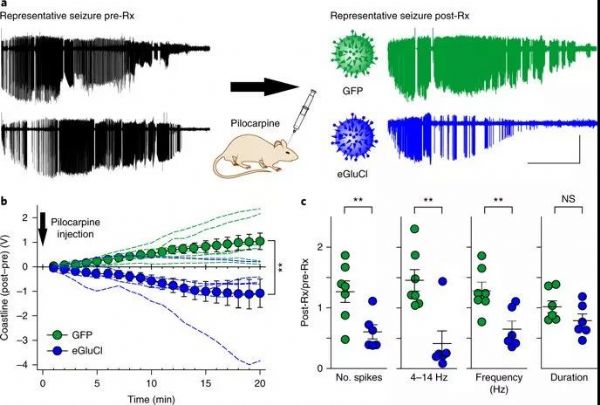
图1. 病毒载体降低了癫痫发作(图片来自原文)
全世界大约有7000万人患有癫痫。尽管在过去20年引入了多种抗癫痫药物,但仍有三分之一的癫痫患者对药物无反应,继续癫痫发作。当癫痫发作来源于大脑特定区域(局灶性癫痫)时,这种耐药性就更加常见。
病毒载体介导的基因治疗有望选择性地修饰引起癫痫发作的神经元群体。这种策略已在不同的动物模型中显示出鼓舞人心的记过,不过,大多数疗法都是不可逆的,因此限制了临床转化。
于是,英国伦敦大学学院神经学研究所的Andreas Lieb及其同事尝试在大鼠身上使用病毒介导的基因疗法,以检测它是否能减少癫痫发作以及耐受性如何。这项研究成果发表在著名期刊《Nature Medicine》上。
Lieb领导的研究团队设计出一种病毒质粒,它包含编码谷氨酸门控氯离子通道的基因。此通道可以检测过量的谷氨酸释放,并以自我调节的方式抑制神经元。在癫痫发作时,谷氨酸释放导致神经活动增强,故抑制这一过程可减少癫痫发作。在慢病毒载体构建过程中,他们选择了赛业生物(Cyagen Biosciences)的服务。
他们首先给成年大鼠注射一种诱发癫痫的药物pilocarpine,然后注射等量的病毒载体或对照载体,且两周后再次注射。这两种载体都注射到大鼠的初级运动皮层。他们将电极置于运动皮层以记录脑电图,从而检测癫痫发作的情况。治疗前后的比较揭示了基因疗法对癫痫发作的作用。
之后,研究人员在慢性局灶性癫痫模型上检测了基因疗法的作用。他们将破伤风毒素注射到大鼠的视觉皮层,几周后大鼠出现癫痫发作。他们同样给大鼠注射病毒载体或对照载体,并通过比较治疗前后癫痫发作的频率来检测治疗效果。
与对照载体相比,大鼠在注射编码谷氨酸敏感通道的病毒载体之后,癫痫发作的频率和幅度都有所降低(图1)。在局灶性癫痫的慢性模型中引入谷氨酸敏感通道后,自发性癫痫发作的频率也降低。
然而,病毒载体对慢性癫痫模型的癫痫发作持续时间没有影响。这些结果表明,基因疗法可有效抑制pilocarpine诱发的癫痫发作相关活动,以及慢性局灶性癫痫发作模型中自发性癫痫发作的次数。
最后,研究人员还开展了一系列行为实验,以检测运动协调是否因基因治疗而改变,即大鼠是否很好地耐受。他们发现对照大鼠和治疗大鼠之间没有差异,表明基因治疗对正常脑功能没有明显影响,具有良好的耐受性。
这项研究第一次证明了基因治疗如何通过表达自我调节的通道来减少癫痫发作。这种基因疗法具有良好的耐受性,能够抑制神经元减少癫痫发作,并减少慢性局灶性模型中癫痫发作的次数。
研究人员表明,基因疗法可用于特定脑部区域的选择性治疗。不过还需要进一步研究,以确保人体对这种基因疗法具有良好的耐受性。
原始出处:Lieb A1, Qiu Y2, Dixon CL2, et al. Biochemical autoregulatory gene therapy for focal epilepsy. Nat Med. 2018 Sep;24(9):1324-1329.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#局灶性癫痫#
87
#Nat#
70
学习了谢谢分享
145
#局灶性#
80
#Med#
74
学习了谢谢分享
112