J Natl Cancer Inst:转移性结直肠癌的一项重要预后因素---原发肿瘤位置
2015-05-04 徐媛媛译 MedSci原创
本研究阐明原发性肿瘤的位置作为转移性结直肠癌(mCRC)的预后因素。 我们评估了肿瘤位置和生存之间的关系参数,将之前未经治疗的转移性结直肠癌并接收一线化疗±贝伐单抗的患者分别来自在三个不同试验:前瞻性PROVETTA研究和两个随机III期研究(AVF2107g,NO16966)。癌症的近端或远端脾曲被分别归类为右或左。以总生存期(OS)为主要结局。利用Cox比例风险和逻辑回归模型作为数据分析模型
本研究阐明原发性肿瘤的位置作为转移性结直肠癌(mCRC)的预后因素。
我们评估了肿瘤位置和生存之间的关系参数,将之前未经治疗的转移性结直肠癌并接收一线化疗±贝伐单抗的患者分别来自在三个不同试验:前瞻性PROVETTA研究和两个随机III期研究(AVF2107g,NO16966)。癌症的近端或远端脾曲被分别归类为右或左。以总生存期(OS)为主要结局。利用Cox比例风险和逻辑回归模型作为数据分析模型。
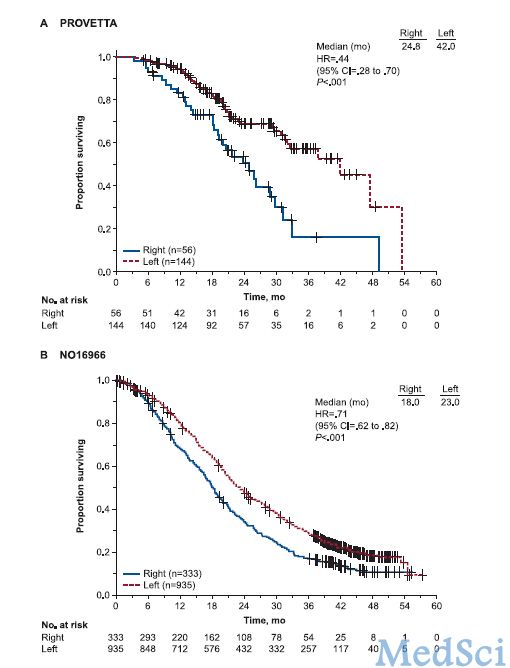
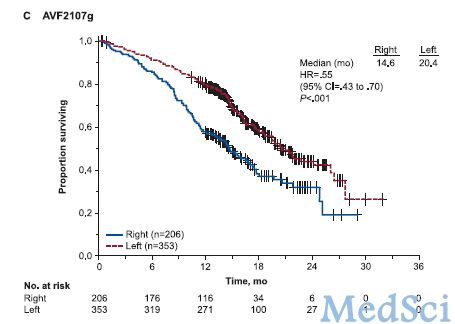
在PROVETTA研究中,收纳200例患者,其中,左侧肿瘤患者占72.0%;在AVF2107g 研究中,患者559例,左侧肿瘤患者占 63.1%;在NO16966研究中,患者1268例,左侧肿瘤患者占73.7%。在PROVETTA试验中,左侧肿瘤患者生存期较长(左侧VS右侧;HR=0.44.95% CI 0.28-0.70,P < .001)和较长的无进展生存期(HR = .52, 95% CI = .36 to .75, P < .001)。经多变量模型证实,左侧原发性肿瘤有较低的进展(HR,0.55;P=0.01)和死亡(HR,0.47;P=0.01)风险,独立于BRAF突变状态或者粘液蛋白组织。研究作者Fotios Loupakis教授(洛杉矶Southern California Norris大学综合癌症中心)在报告中说。在AVF2017g(HR for OS = .55, 95% CI = .43 to .70) 和 NO16966 (HR for OS = .71, 95% CI = .62 to .82 both P < .001) 试验左侧肿瘤无进展生存期明显更长。多变量分析证明无论患者接受贝伐珠单抗治疗与否,肿瘤位置的预后影响具有独立性。
以上数据表明,在之前未经治疗的转移性结直肠癌患者中,原发肿瘤的位置是一项重要的预后因素。考虑到结果的一致性和两个III期研究,在未来的随机试验中,可以将肿瘤位置作为一个重要分层因素进行考虑。
原始出处
Loupakis F1, Yang D1, Yau L1, Feng S1, Cremolini C1, Zhang W1, Maus MK1, Antoniotti C1, Langer C1, Scherer SJ1, Müller T1, Hurwitz HI1, Saltz L1, Falcone A1, Lenz HJ2.Primary tumor location as a prognostic factor in metastatic colorectal cancer.J Natl Cancer Inst. 2015 Feb 24;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ATL#
85
#NST#
82
#肿瘤位置#
103
#Nat#
88
#原发肿瘤#
100
#转移性#
77
#结直肠#
83
#预后因素#
85