Nat. Rev. Endocrinol.: PCSK9或为降低LDL胆固醇新靶点
2013-05-27 Nat. Rev. Endocrinol dxy
关键进展: 抑制前蛋白转化酶枯草杆菌酶/kexin 9(PCSK9)的单克隆抗体可减少LDL-胆固醇水平 靶向PCSK9抗体能降低家族性或原发性高胆固醇血症患者LDL胆固醇水平,与他汀类药物疗效叠加 靶向PCSK9抗体降低他汀类药物不耐受的患者的LDL胆固醇水平 抗PCSK9抗体全身给药显著降低LDL胆固醇水平,该疗法对LDL胆固醇受体活性的作用与他汀类药物的作用具有叠加
关键进展:
- 抑制前蛋白转化酶枯草杆菌酶/kexin 9(PCSK9)的单克隆抗体可减少LDL-胆固醇水平
- 靶向PCSK9抗体能降低家族性或原发性高胆固醇血症患者LDL胆固醇水平,与他汀类药物疗效叠加
- 靶向PCSK9抗体降低他汀类药物不耐受的患者的LDL胆固醇水平
抗PCSK9抗体全身给药显著降低LDL胆固醇水平,该疗法对LDL胆固醇受体活性的作用与他汀类药物的作用具有叠加效应。抑制PCSK9对临床医生来说具有潜在的重要性,并且应该能使更多患者LDL胆固醇达标。
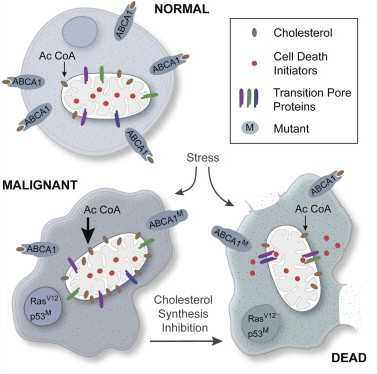
20世纪80年代晚期,他汀类药物的临床应用改变了心血管疾病(CVDs)的治疗。这类药物能够抑制胆固醇合成过程中的限速酶,即HMG-CoA还原酶。由于这种抑制作用,肝脏表达的LDL受体(LDLR)含量增加,血浆LDL胆固醇水平降低。他汀类药物耐受性较好,可有效降低CVD患者LDL胆固醇水平。它的成功应用使得更多评价这类药物用于冠心病事件一级和二级预防的随机安慰剂对照临床试验得以进行。现已有大量的有效性和安全性方面的数据指导CVD风险增高相关疾病的治疗。此外,使用高剂量他汀类或强效他汀类药物强化降LDL胆固醇,CVD风险降低程度较使用低剂量他汀类或弱效他汀类药物显著提高。
他汀类药物被推荐作为降低LDL和其它含载脂蛋白B-100脂蛋白水平的一线治疗药物。在过去十年中,治疗目标变得更加严格。对于CVD 极高危患者,推荐LDL胆固醇目标水平<1.8mmol/l。在2型糖尿病或其它与混合型脂质血症相关疾病的患者中,考虑到除LDLs脂蛋白外,致动脉粥样胆固醇还可能存在于其它类型脂蛋白中(如中密度脂蛋白和残留颗粒),主张非HDL胆固醇水平<2.6mmol/l作为次要治疗目标。
尽管他汀类药物在临床上广泛使用,要使LDL胆固醇降低到目标水平仍然具有一定的挑战。例如,以下患者的LDL胆固醇则难以达标:因为严重的原发性血脂障碍(例如家族性高胆固醇血症,家族联合性高脂血症或Ⅲ型β脂蛋白异常),基线LDL胆固醇水平非常高的患者; 极高CVD 风险、需要强化治疗的患者;由于潜在严重药物相互作用、合并症或不能耐受高剂量他汀类药物而导致的他汀类药物剂量受限的患者。此外,一些患者因为多种原因不能或不愿服用他汀类药物,在多个脂质门诊中,这个问题代表了主要的转诊模式。他汀类药物不耐受的患者的比例难以确定,但是以我作为一个临床医生的经验来说,这个比例大约为10%。因此,尽管现有的他汀类药物是任何一个医学分支中最重要的发明之一,仍然有大量的患者使用该类药物后达不到治疗目标。在过去十年中,所取得的令人振奋的进步是,遗传突变影响胆固醇代谢的详细研究鉴定了新的治疗靶点。丝氨酸蛋白酶前蛋白转化酶枯草杆菌酶/kexin 9(PCSK9)正是这样一个例子。
肝脏LDLRs活性是血浆LDL浓度的主要决定因素,一项对严重家族性高胆固醇血症表型的研究鉴定了一个先前未知的细胞生理过程,这个过程对LDLR活性具有重要性。PCSK9是一个丝氨酸蛋白酶,主要在肝脏合成,它能够减少肝细胞中LDLRs数量。循环中PCSK9与位于细胞表面的LDLR结合后,内化至细胞里,促进溶酶体中LDLR降解。因此,PCSK9的活性升高导致LDLR数量减少,血浆中LDL水平增高。PCSK9获得功能性突变产生严重家族性高胆固醇血症表型,而缺失功能性突变与出生时血浆LDL浓度降低和CVD风险降低有关。有趣的是,他汀类药物治疗期间,PCSK9水平增加。
鉴定PCSK9对LDLR活性调节方面的研究为干预治疗带来了新靶点。能反应其重要性的是PCSK9 抑制剂Ⅰ期及随后的Ⅱ期临床研究结果均已发表在今年几个较为重要的杂志上。靶向PCSK9的特异性抗体与PCSK9结合,阻断它与LDLR的相互作用。多个Ⅰ期临床单剂量研究对两个不同的特异性人单克隆抗体制剂REGN727/SAR236553(REGN727)和AMG145在健康人体中的作用进行了评价,研究的阳性结果表明这种治疗方法的巨大潜力,抗体治疗组LDL胆固醇水平较安慰剂对照组降低约60%。抗PCSK9抗体的作用效果和持续时间呈剂量依赖性,剂量越高,作用时间越长,LDL胆固醇水平降低程度越大。
在两项为期12周的随机双盲安慰剂对照Ⅱ期临床试验中,对REGN727不同剂量和不同给药间隔的有效性和安全性进行了评价。其中一项研究纳入77名接受他汀类药物治疗的杂合型家族性高胆固醇血症患者,另一项研究纳入183名接受他汀类药物治疗的原发性高胆固醇血症患者。家族性高胆固醇血症患者在他汀类药物治疗的基础上给予150mg的REGN727,每两周一次。结果显示,REGN727添加到他汀类药物中可降低LDL胆固醇水平(67.9%)和载脂蛋白B-100 (一个主要的携带致动脉粥样硬化胆固醇的蛋白)水平(50.19%)。同时,载脂蛋白A-I(主要的HDL蛋白)和HDL胆固醇水平分别增加8.82%和12.34%。REGN727潜在的作用机制仍有待确定,但是这些结果提示,经胆固醇酯转移蛋白介导的胆固醇酯从HDL到LDL的转移率降低。Mckenney等的研究结果与上述情况类似,虽然HDL胆固醇水平和载脂蛋白A-I在REGN727治疗后降低。要解释这两个研究结果之间的差异具有一定的困难,而且在这种情况下可能不太适当,因为两个研究的样本量较少,且研究周期短。单克隆抗体添加到他汀类药物中具有疗效叠加的效果,而不是协同作用。经他汀类药物治疗的患者PCSK9水平增加,由此可以预见,当PCSK9被抑制后,将会观察到更多的叠加效应,但是事实上这样的反应没有观察到。
明显地,这种新的疗法对于他汀类药物不耐受的患者来说具有很大的益处,这类人群被纳入“他汀类不耐受患者使用抗PCSK9抗体后达到治疗目标(GAUSS)临床试验”研究。由于肌痛或肌病,将不能耐受他汀类药物的患者随机分配接受单克隆抗体抗PCSK9抗体AMG145或安慰剂治疗12周,每4周给药一次,单独使用或联合应用依泽替米贝(10mg/天)。结果显示,AMG145的作用呈剂量依赖性,高剂量(420mg)组LDL胆固醇最高降低51%。AMG145与依泽替米贝联合具有疗效叠加效应,AMG145(420mg)和依泽替米贝 (10mg/天)联合治疗后LDL胆固醇降低63%。在不耐受他汀类的患者中,LDL胆固醇降低具有显著性,这种方法应该可有效治疗该组患者。
2012年发表的关于这些单克隆抗体的早期疗效数据令人印象非常深刻,但是到目前为止这些研究周期较短,样本量小。在这些药物被批准上市和进入临床使用之前,仍需要长期有效性和安全性数据。我们用于考察降脂疗法的一般安全性数据看起来鼓舞人心,但是与单克隆抗体有关的潜在安全性问题是什么?一项对原发性高脂血症患者的研究中,一名57岁的男性接受初始剂量为300mg 的REGN727治疗后出现腹泻,然后是皮疹,经组织活检诊断为白细胞破裂性血管炎。这种普遍的良性疾病在接受其它抗体治疗的患者中也已报道。
另一个需要考虑的问题是,注射部位轻微反应是否影响患者的顺应性。间隔2-4周的皮下注射给药方式容易被患者接受吗?当然,2型糖尿病患者似乎都能接受GLP-1激动剂皮下注射给药。另一个决定这些药物给药频率的影响因素是这种治疗方法的费用:效益比(由健康护理提供者评价)。可以想象得到,大多数的提供者能接受这类药物用于治疗那些经最大剂量他汀类药物和依泽替米贝治疗后LDL胆固醇仍不能达标的严重脂质障碍患者。但是,在允许使用单克隆PCSK9抗体之前,护理提供者会要求患者符合确切的他汀类药物不耐受的定义吗?我们应怀着极大的兴趣跟踪这一新的治疗领域的发展。

Cardiovascular endocrinology in 2012: PCSK9-an exciting target for reducing LDL-cholesterol levels.
Abstract
Systemic administration of anti-PCSK9 antibodies induces dramatic reductions in LDL-cholesterol levels, and the effect of this therapy on LDL-receptor activity seems to be additive to that of statin therapy. Inhibition of PCSK9 is potentially very important to the clinician, and should enable more patients to achieve their LDL-cholesterol-level goal.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PCS#
97
#Nat#
101
#Csk#
74
#LDL胆固醇#
85
#新靶点#
104
#LDL#
77