Nat Commun: 内皮激活素A与骨形态发生蛋白受体2型链接在肺动脉高压中作用
2021-11-04 刘少飞 MedSci原创
肺动脉高压是一种进行性致命疾病,其特征是病理性肺动脉重塑,其中严重涉及内皮细胞功能障碍。内皮细胞过量产生抑制素-β-A通过作为激活素-A 起作用以自分泌方式损害内皮功能。该研究将探讨激活素-A的作用。

An endothelial activin A-bone morphogenetic protein receptor type 2 link is overdriven in pulmonary hypertension.
研究内容:
肺动脉高压是一种进行性致命疾病,其特征在于病理性肺动脉重塑,其中严重涉及内皮细胞功能障碍。研究在此描述了内皮细胞所分泌的物质在肺动脉高压中以前未知的作用。通过分析在肺微血管内皮细胞中高度表达的基因,研究确定抑制素-β-A是肺毛细血管产生的内分泌因子,而且发现内皮细胞抑制素-β-A的过量生产是通过激活素-A的功能以自分泌方式损害了内皮功能。从机制上讲,激活素A诱导BMPR2靶向溶酶体进行降解,从而导致内皮细胞BMP信号不足。值得注意的是,与从正常对照受试者的肺中分离出的内皮细胞相比,特发性肺动脉高压患者的肺中分离出的内皮细胞显示更高的抑制素-β-A表达,并产生更多的激活素-A。当小鼠中的内皮细胞BMPR2被激活素-A过度降解时,缺氧诱导的肺动脉高压加剧,而内皮细胞中抑制素-β-A的条件性敲除阻止了肺动脉高压的发展。这些数据共同表明,在肺动脉高压的进展中,肺动脉高压进展中内皮细胞激活素-A-骨形态发生蛋白受体2型失调起到重要作用,内皮抑制素-β-A/激活素-A可能是治疗肺动脉高压的潜在药物治疗靶标。
研究结果:
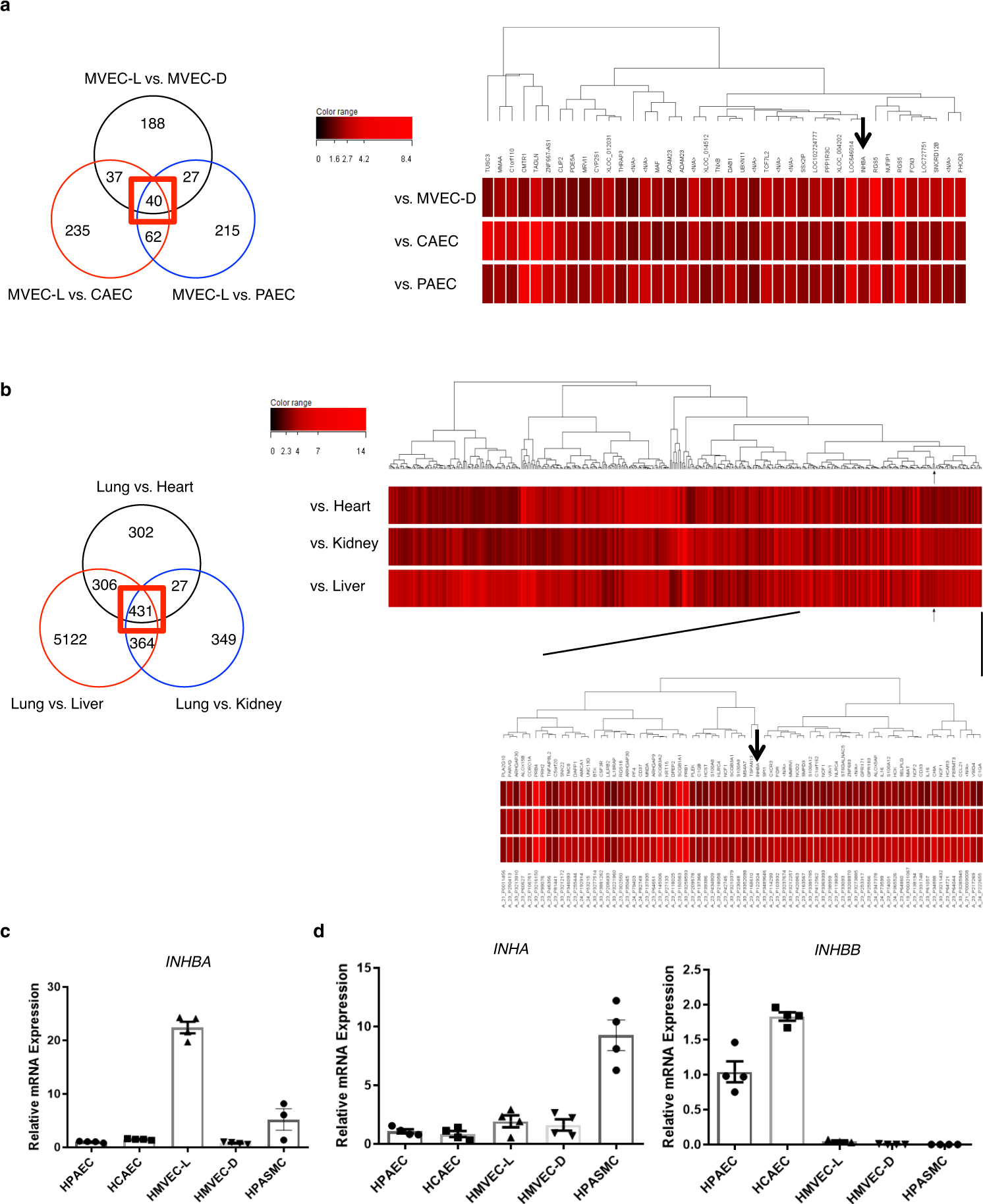
通过从分离自各种血管床的人类EC制备的RNA和从各种人体组织制备的RNA,DNA微阵列分析高度优先表达于肺微血管EC(hMVECs-L)中的基因,从而鉴定出抑制素-β-A(INHBA)作为在肺微脉管系统中高表达的基因。
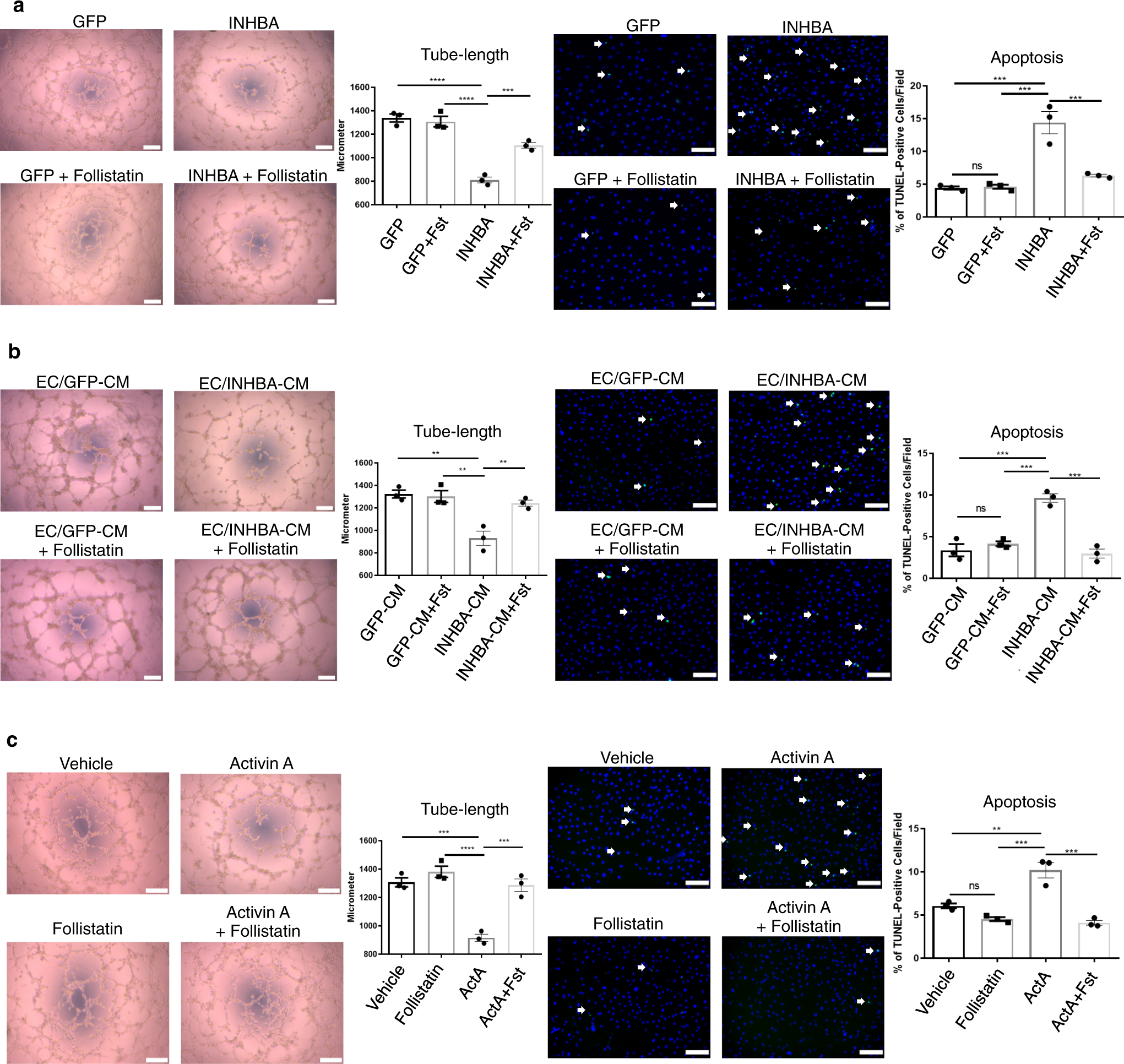
为了探索INHBA/ActA在EC中的作用,在PAEC中过表达了INHBA,并分析了它们的血管生成能力。结果发现过量的INHBA /ActA介导的血管分泌抑制PAECs的血管生成能力。
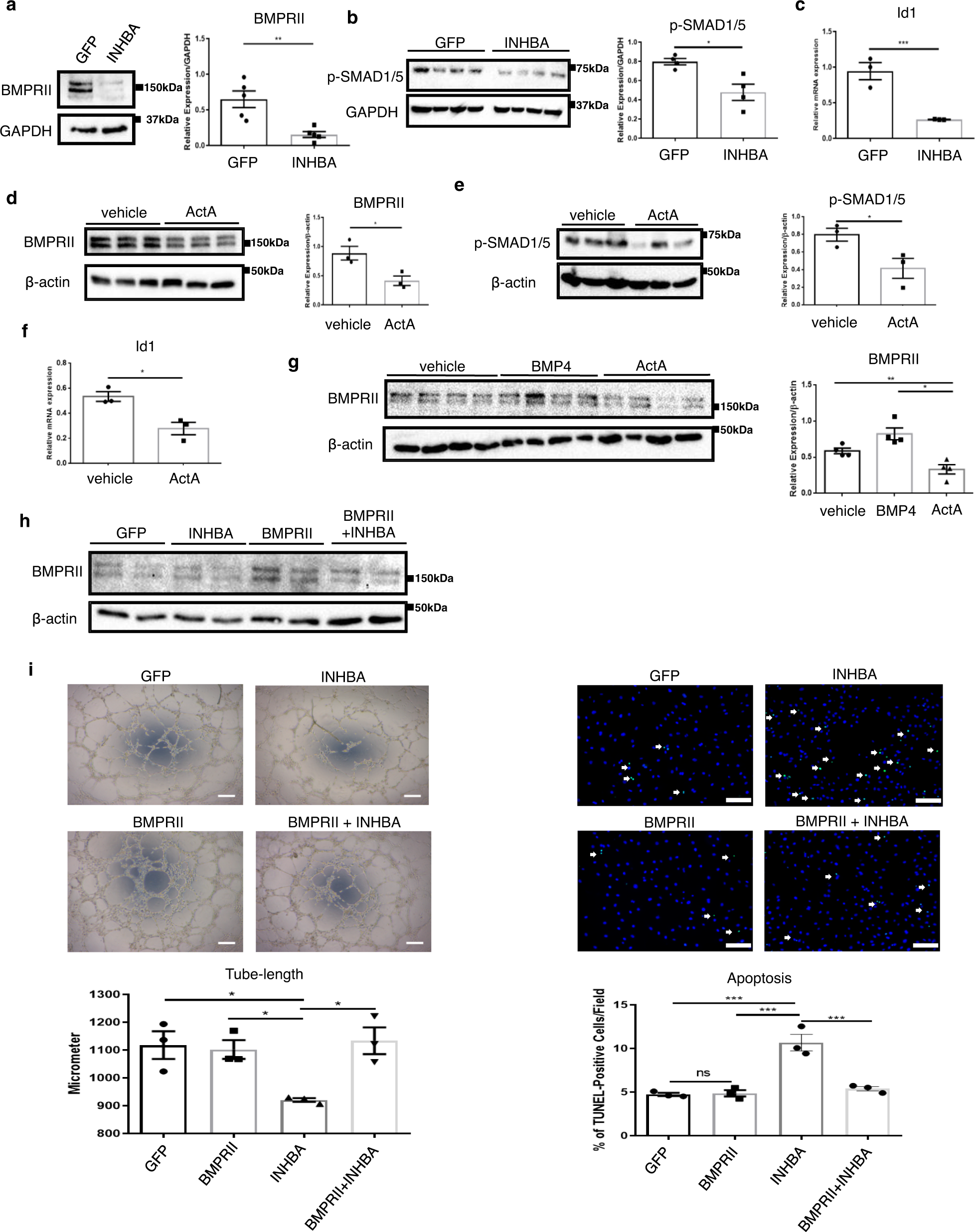
由于ActA具有与BMPRII结合的能力,而BMPRII信号对于维持EC功能(尤其是在肺血管系统中)至关重要,因此该研究考虑BMPRII信号作为INHBA / ActA介导的EC功能障碍的可能中介机制。结果展示INHBA / ActA过多会降低BMPRII,从而损害EC功能。
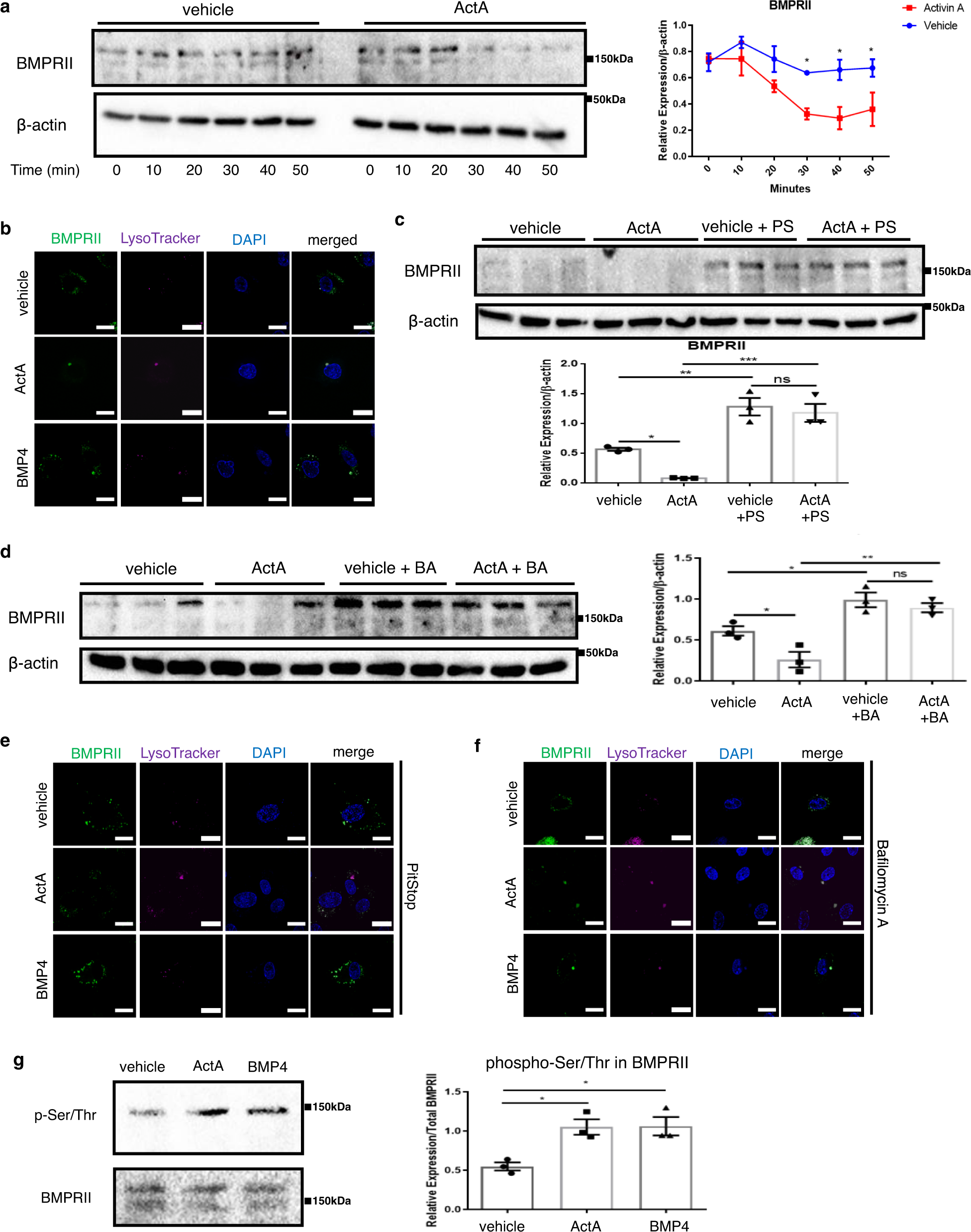
许多受体主要通过网格蛋白介导的内吞作用经历配体诱导的内在化,其中一些受体循环回到细胞膜,而另一些则靶向降解。尽管mRNA的表达变化很小,但由于INHBA/ActA降低了BMPRII蛋白的水平,因此我们推测INHBA / ActA可能会增强BMPRII蛋白的降解。研究发现ActA加速配体介导的BMPRII内吞和溶酶体降解。
ECs中INHBA的靶标激活会加剧BMPRII信号传导,进而加重PH。
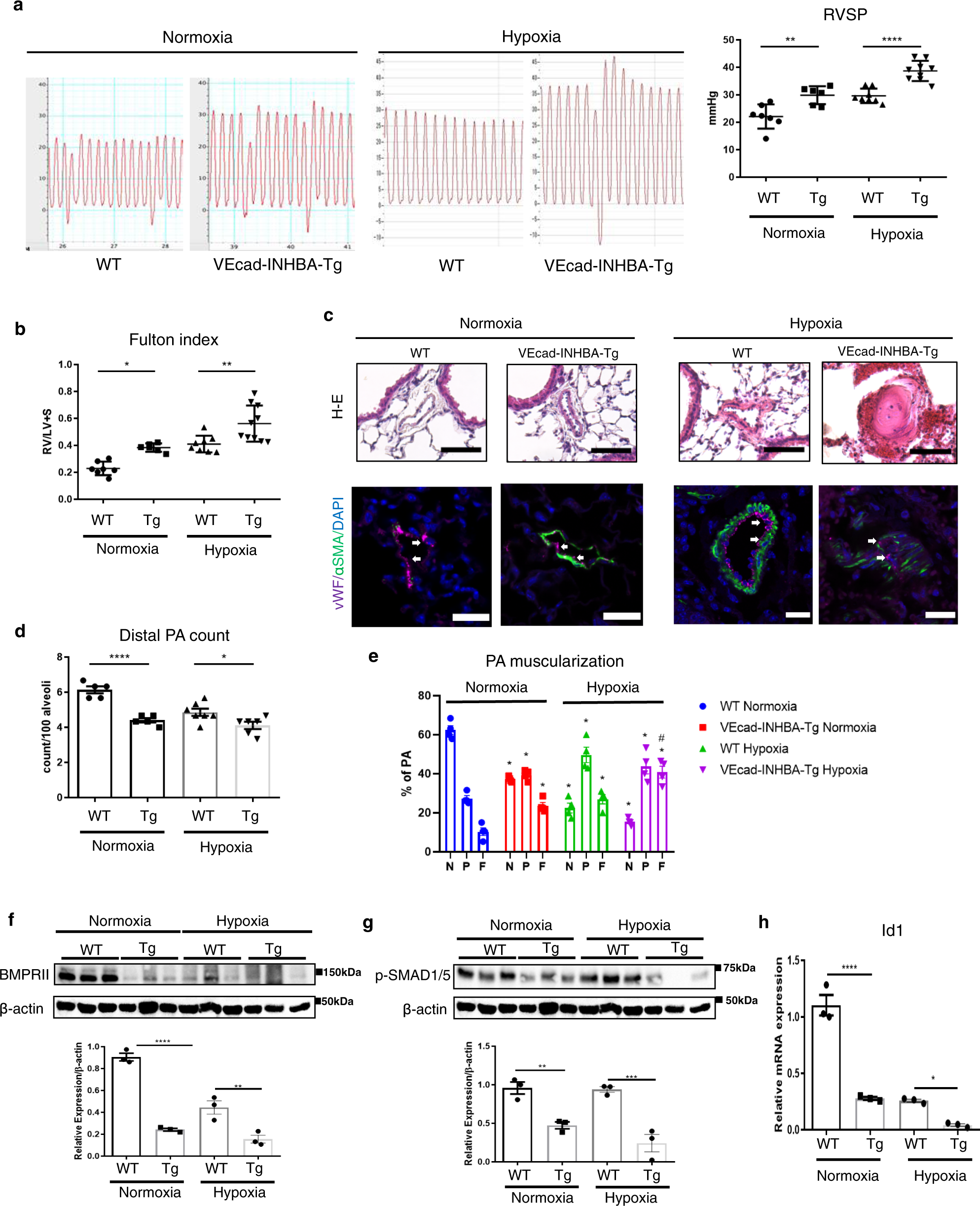
EC特异性的INHBA缺失可改善小鼠低氧诱导的PH;而且从特发性肺动脉高压患者中分离出的肺EC中,INHBA/ActA的表达过高。

研究结论及展望:
尽管已证明BMPRII活性保留在预防和逆转血管方面很重要。在PAH中重塑,临床上尚未建立恢复BMPRII表达的治疗选择。该研究数据表明,ActA介导的血管分泌可能是恢复BMPRII功能的有希望的治疗靶标。在这方面,卵泡抑素(ActA的内源性抑制剂)是治疗PAH44的良好候选药物。然而,它拮抗诸如肌肉生长抑制素的各种TGF-β超家族成员,实际上,关于杜氏肌营养不良症,其临床应用已得到深入研究。开发针对ActA的配体陷阱(基于卵泡抑素)将构成PAH治疗方面的突破。实际上,Sotatercept是一种对包括ActA在内的TGF-β超家族的多个成员具有高选择性的配体陷阱,目前已经结束了PAH患者中2期临床试验。时隔六年,又一重大发现发表于《新英格兰杂志》: Sotatercept用于治疗肺动脉高压。INHBA / ActA介导的肺微血管血管分泌是PAH发育过程中一个未知的修饰因子。有必要进行进一步的临床研究,以确认INHBA / ActA是治疗PAH的治疗靶标
文章出处:
Ryanto GRT, Ikeda K, Miyagawa K, Tu L, Guignabert C, Humbert M, Fujiyama T, Yanagisawa M, Hirata KI, Emoto N. An endothelial activin A-bone morphogenetic protein receptor type 2 link is overdriven in pulmonary hypertension. Nat Commun. 2021 Mar 19;12(1):1720. doi: 10.1038/s41467-021-21961-3. PMID: 33741934; PMCID: PMC7979873.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#激活素A#
75
#骨形态发生蛋白#
0
#COMMUN#
64
#Nat#
62
#动脉高压#
90
学习了,谢谢分享
84