Hypertension:视网膜血管形态与血压、动脉僵硬度指数的相关性
2019-11-17 QQY MedSci原创
为研究视网膜血管形态与血压(BP)和动脉硬化的相关性,英国生物库对68 550名40到69岁的受试者予以非扩瞳视网膜成像、BP和动脉僵硬指数评估。一个全自动的图像分析程序提供了视网膜血管直径和弯曲度的测量数据。采用多层线性回归模型分析视网膜血管形态与心血管疾病危险因素/预后的相关性,并根据年龄、性别、种族、临床、体重指数、吸烟和剥夺指数进行调整。细动脉扭曲越明显,收缩压越高(相对增加1.2%;[9
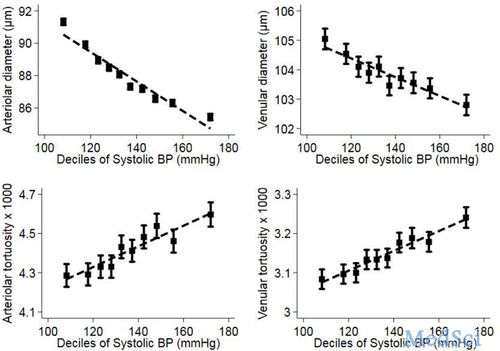
细动脉扭曲越明显,收缩压越高(相对增加1.2%;[95%CI 0.9-1.4%/10mmHg]),平均动脉压和脉压也更高(1.3% [0.9-1.7%/10mmHg];PP 1.8%[1.4-2.2%/10mmHg])。细动脉越细,收缩压、平均动脉压和动脉僵硬指数越高。静脉扭曲极其直接与血压的相关性与动脉的相似,但相关性较弱。
总而言之,本研究表明视网膜血管形态与血压和动脉僵硬度指数之间存在明显的相关性。该结果进一步加深了我们对微血管和大血管疾病的临床前病变过程和相互作用的理解。
原始出处:
Robyn J. Tapp, et al.Associations of Retinal Microvascular Diameters and Tortuosity With Blood Pressure and Arterial Stiffness.Hypertension. 2019;74:1383–1390
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
92
#TENS#
108
#PE#
98
#视网膜#
71
#Hypertension#
98
#动脉僵硬#
84
#动脉僵硬度#
68