JCO:溶瘤病毒T-VEC对晚期恶性黑色素瘤有持久的保护效应
2015-05-27 何嫱 生物通
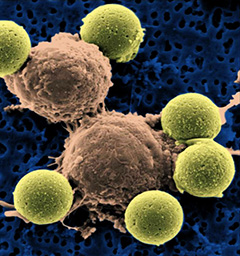
一项具有里程碑意义的临床试验证实,一种遗传工程疱疹病毒可通过杀死癌细胞,激发免疫系统发挥作用来对抗肿瘤,抑制皮肤癌病情的发展。这是全球第一次,一项III期病毒免疫治疗试验明确显示让癌症患者获益。来自英国癌症研究所、皇家Marsden NHS基金会,和包括牛津大学在内全球64家研究中心的研究人员共同领导了这项试验。研究人员随机选择436名罹患侵袭性恶性黑色素瘤、无法接受手术治疗的患者接受了一种叫做T
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#色素#
61
#JCO#
76
#T-VEC#
63
看看
176
#黑色素#
60
#黑色素#
54
真正意义上的病毒药物,不像国内的太虚
163