AP&T: 饮酒量和炎症性肠病发病风险存在相关性
2022-01-11 MedSci原创 MedSci原创
炎症性肠病(IBD)为累及回肠、直肠、结肠的一种特发性肠道炎症性疾病。 炎症性肠病(IBD)为累及回肠、直肠、结肠的一种特发性肠道炎症性疾病。
克罗恩病(CD)和溃疡性结肠炎(UC),统称为炎症性肠病(IBD)。他们是一种渐进性、免疫性胃肠道炎症疾病。尽管免疫反应和肠道微环境在这两种疾病的发展中的作用已经确定,但IBD的确切病因尚不清楚。然而,一些环境风险因素已经被确认,包括饮食、使用非甾体抗炎药物(NSAIDs)、吸烟和压力等。已知从酒精饮料中摄入的乙醇会损害肠道屏障功能和渗透性,此外,饮酒也与促炎症途径有关。具体来说,短期饮酒可以降低T细胞活性,而长期饮酒会增加TNF-ɑ、白细胞介素-1和白细胞介素-6等炎症因子的释放。尽管有这些观察,但关于饮酒和IBD风险之间关系的高质量流行病学研究有限。为此,本项研究进行了全面的饮酒与CD和UC风险之间的关系的探究。

研究人员对来自美国护士健康研究、护士健康研究 II 和健康专业随访研究的 237,835 名参与者进行了前瞻性队列研究。通过每四年提交一次问卷调查获得所有受试者的酒精消耗量;每隔两年或四年获得额外的一些统计数据。病例由两名医师通过病历审查独立确认。最后使用 Cox 比例风险回归来估计年龄和多变量调整风险比和 95% 置信区间。

研究结果显示在 5,170,474 人年的随访时间中,总共记录了 370 例 CD 和 486 例 UC的发生。酒精摄入量增加与 CD (P= 0.455) 或 UC (P= 0.745) 无关。与非使用者相比,大于15.0g/天酒精摄入组的HR分别为: CD 为0.84(95% CI 0.56, 1.24)和 UC为 1.08(95% CI 0.77, 1.51)。在对酒精亚型的分析中,研究人员观察到,只有适度饮用啤酒(>1-4 份/周)与 CD 风险降低略有相关,而每周饮用>4 份酒与 UC 风险增加相关.
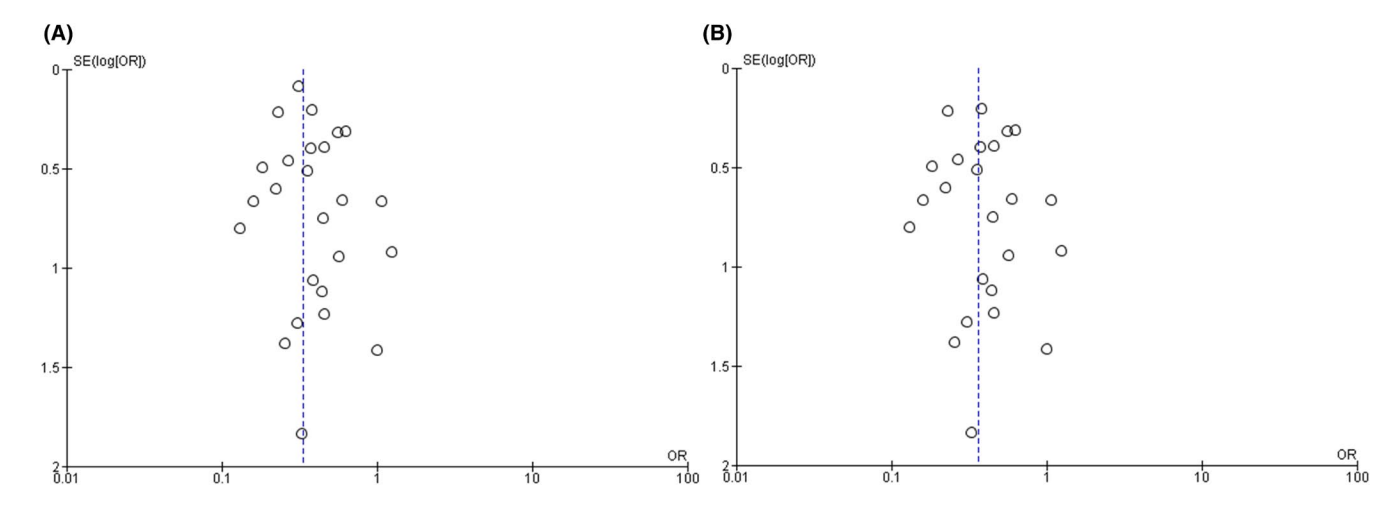
图:CD与UC患者饮酒时随时间变化的发生率变化
本项研究虽然没有确定总体饮酒量与 CD 或 UC 风险之间的关系,但对酒精类型与 CD 和 UC 风险之间潜在关系值得进一步探究。
原始出处:
Kevin Casey. Et al. Alcohol consumption and risk of inflammatory bowel disease among three prospective US cohorts.Alimentary Pharmacology & Therapeutics.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
70
#饮酒量#
96
期待继续继续相关研究
0
学习了
97
学习了
84
#炎症性#
71