Front Med:在接受免疫治疗的受试者中,病毒性肝炎重新激活的低发生率减少了次优筛查率的影响
2022-08-11 从医路漫漫 MedSci原创
ICIs免疫疗法基于使用针对检查点分子的单克隆抗体,促进免疫系统的激活并诱导转移细胞的消除。
背景:免疫检查点抑制剂(ICIs)已成为许多晚期癌症治疗的突破。ICIs免疫疗法基于使用针对检查点分子的单克隆抗体,促进免疫系统的激活并诱导转移细胞的消除。最常用的机制是细胞毒性T淋巴细胞相关分子-4(抗CTLA-4)、程序性细胞死亡受体-1(抗PD-1)、程序性细胞死亡配体-1(抗PD-L1)和抗LAG3。迄今为止,ICIs免疫疗法已被批准用于超过17种不同类型的癌症,并且正在发展。众所周知,化疗存在乙肝病毒(HBV)再激活的风险,尤其是在血液学领域。此外,慢性丙型肝炎在患有一些实体器官肿瘤(如肝细胞癌和非霍奇金淋巴瘤)的受试者中更为普遍。然而,病毒性肝炎筛查在化疗候选人中并不普遍,这一事实导致了电子警报和平台的发展,以促进开化疗处方的医生的诊断。这些措施是基于HBV再激活患者的发病率和死亡率预后较差。与化学疗法不同,关于免疫疗法对病毒性肝炎的疗效的数据很少,关于开处方的医生对这一主题的认识的信息也很缺乏。在大多数ICIs的注册研究中,患有潜在病毒性肝炎的个体被排除在外,或者在慢性HBV患者的情况下,至少需要接受核苷(酸)类似物(NAs)治疗。来自真实世界队列的回顾性研究表明,在没有抗病毒预防的免疫治疗情况下,高达17%的HBV感染受试者可能遭受再激活。关于已解决的HBV感染(分离的抗-HBc+受试者),到目前为止报道的再激活病例很少,尽管关于再激活的真实发生率的数据仍然未知。与HBV相反,丙型肝炎病毒载量似乎没有改变,甚至减少了ICIs的影响。
目的:本研究的目的是在开始ICIs前分析乙型和丙型肝炎的检测率,作为评估肿瘤学家对接受免疫治疗人群中病毒性肝炎认识的一种方法。此外,我们前瞻性地评估了接受免疫治疗的患者中病毒性肝炎的患病率以及在这种情况下病毒性肝炎再激活的潜在风险。
方法:回顾性-前瞻性研究,包括2019年1月至2020年12月在大学医院开始ICIs的所有患者。收集ICIs开始前的病毒性肝炎筛查数据。在缺乏信息的受试者中,前瞻性地要求进行血清学试验。在HBsAg、抗-HBc或抗-HCV阳性受试者中,对再激活进行前瞻性评估。
结果:在2年的研究期间,595名受试者接受了ICIs (61.2%为男性,平均年龄63岁)。发现的最普遍的癌症是35.5%的肺癌、12.1%的黑色素瘤和8.2%的头颈癌;ICIs方案主要是抗PD1 (65.7%),其次是抗PD-L1 (19.2%)和联合治疗(13.6%)。在免疫治疗之前,462名(77.6%)受试者进行了抗-HCV筛查,462名(77.6%)受试者进行了HBsAg筛查,335名受试者进行了抗-HBc筛查(56.3%),328名受试者进行了全面筛查(55.1%)。在接受合并全身治疗的患者中,抗-HBc筛查更频繁(p = 0.003),尤其是在化疗的情况下(p = 0.015),尽管HCV筛查在不同于化疗的合并治疗中更常见(p = 0.001)。在存活者中前瞻性地完成了血清学检测,导致抗-HCV总患病率为3.5%,HBsAg为1.3%,抗-HBc为15.2%。在2/19(均为肝细胞癌患者)中检测到HCV-RNA,在4/7 HBsAg阳性和1/75抗-HBc阳性受试者中检测到HBV-DNA。7名HBsAg携带者中的5名和1/75名抗HBc+受试者(由于伴随抗逆转录病毒治疗)接受了抗病毒预防。既没有观察到HBV再激活的病例,也没有观察到HCV病毒载量的变化。
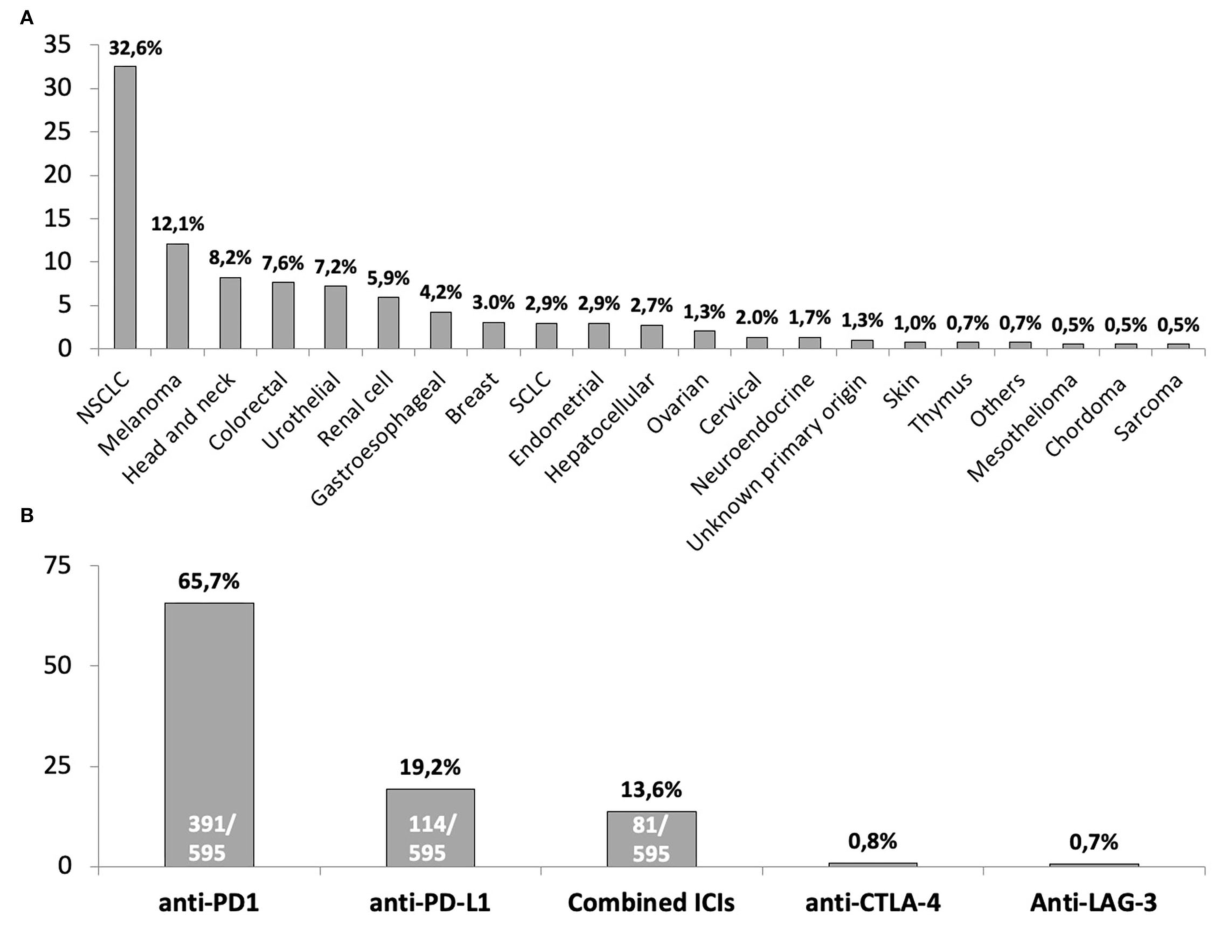
图1 |免疫检查点抑制剂治疗的潜在癌症总结(A)和为纳入患者开出的免疫检查点抑制剂方案(B)。NSCLC,非小细胞肺癌;小细胞肺癌。“其他”肿瘤类别中的四名(0.7%)受试者包括:1例副神经节瘤、1例孤立性纤维性肿瘤、1例甲状腺、1例霍奇金淋巴瘤。在用抗CTLA-4或抗LAG-3进行单一治疗的情况下,接受这些ICIs方案的受试者的绝对数量分别为5和4。
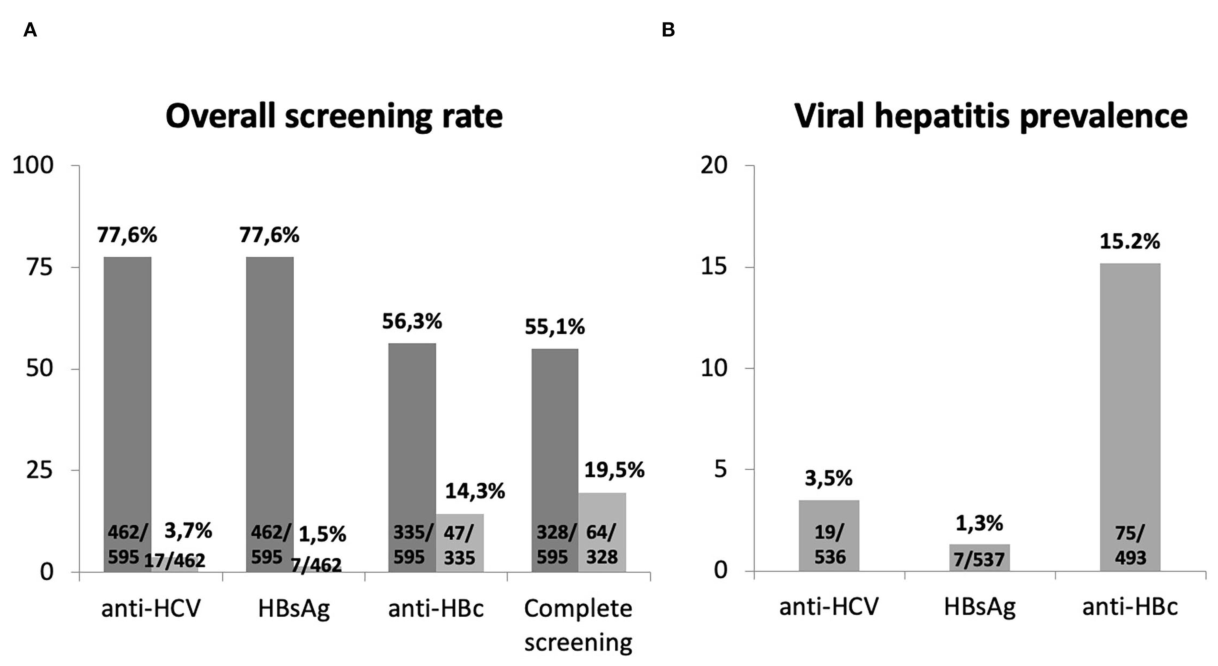
图2 | (A)在ICIs开始前(深灰色)订购的病毒性肝炎标志物的比率和这些测试的结果(浅灰色)。(B)在ICIs存活患者中预期要求病毒性肝炎标志物后的总体病毒性肝炎患病率。完整的病毒性肝炎检测是指结合HBsAg、抗-HBc和抗-HCV
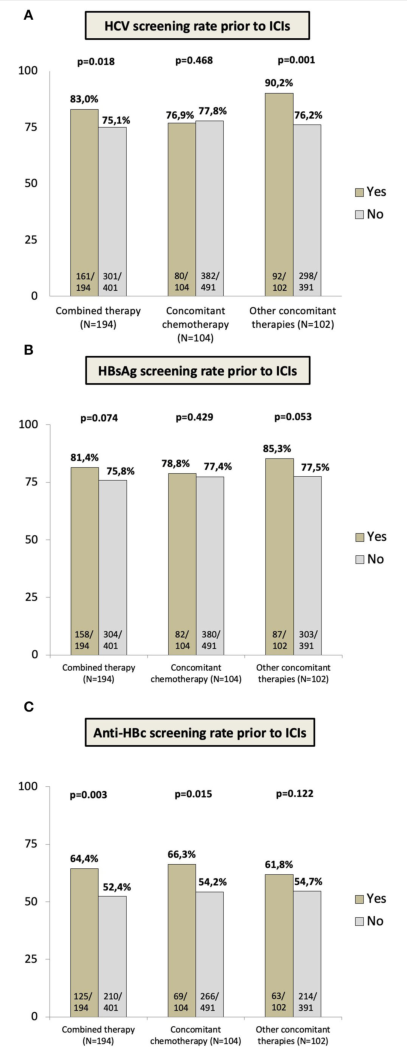
图3 |根据合并用药(所有联合治疗)的处方,在ICIs开始前要求进行病毒性肝炎检测的比率;伴随化疗;不同于化疗的伴随全身治疗,主要是酪氨酸激酶抑制剂、IL-2激动剂、诱导型共刺激因子-ICOS和抗VEGF药物,如补充表1中所总结的:(ICIs前的丙型肝炎病毒筛查。(二)ICIs前的HBsAg筛查。(C)在ICIs之前进行抗HBc筛查。
结论:在免疫治疗前进行HBV和丙肝病毒筛查是不理想的。尽管病毒性肝炎再激活率似乎极低,但在选择抗病毒预防或定期随访的候选人进行免疫治疗前,应努力优化病毒性肝炎筛查。
原文出处:Aceituno L, Bañares J, Ruiz-Ortega L,et al.The Low Incidence of Viral Hepatitis Reactivation Among Subjects on Immunotherapy Reduces the Impact of Suboptimal Screening Rate.Front Med (Lausanne) 2022;9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
111
#病毒性#
99
#重新激活#
102
#受试者#
96
#Med#
74