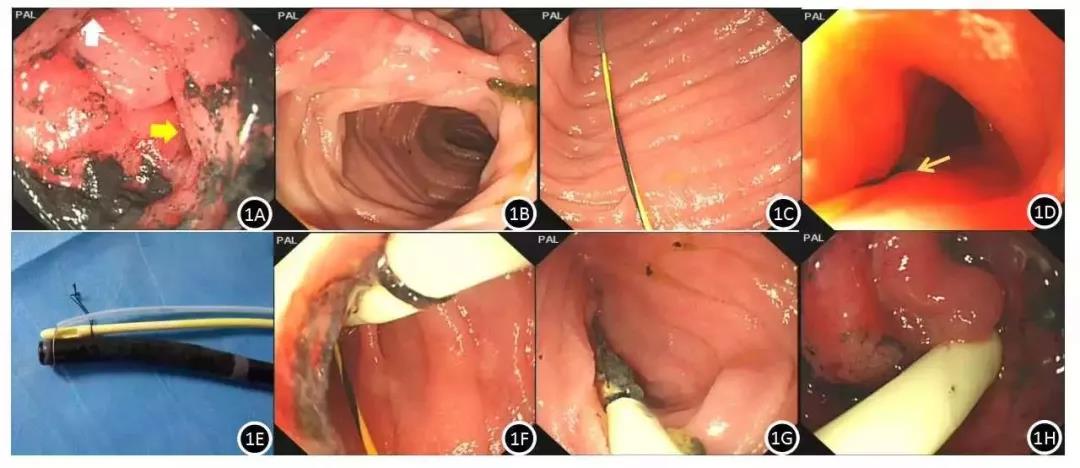
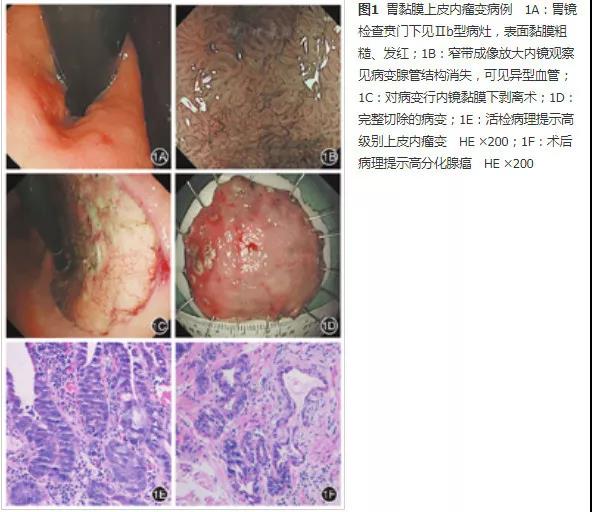
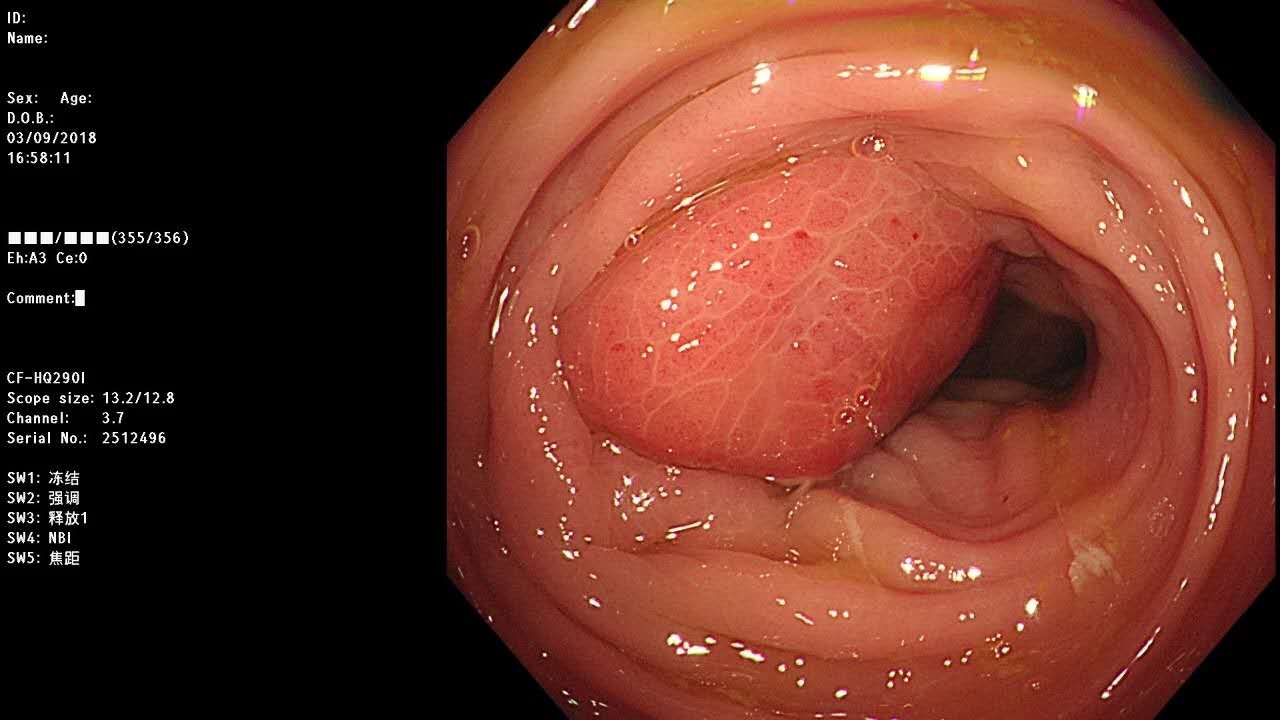
病例:内镜下切除食管下段巨大平滑肌瘤
2019-03-30 青海涛 消化专家青海涛大夫
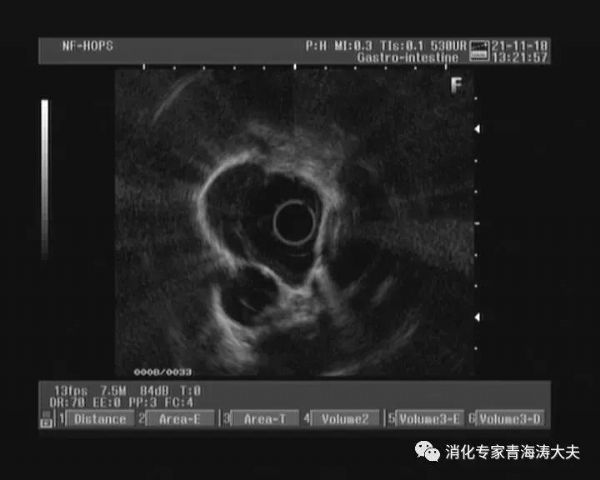
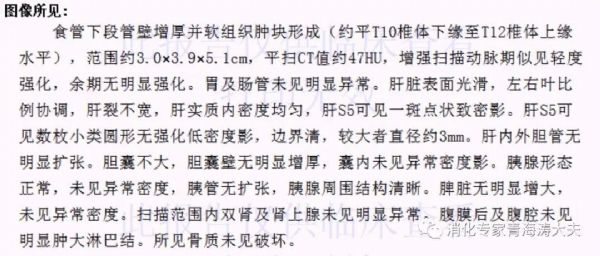
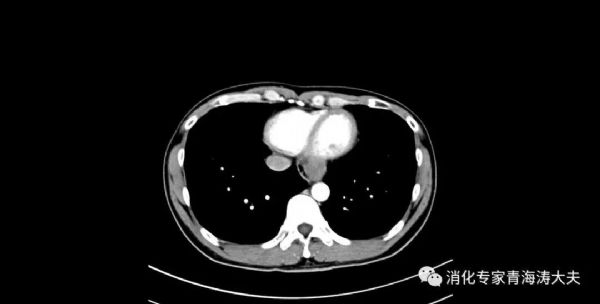
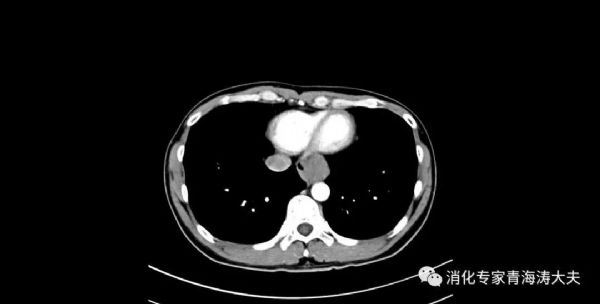
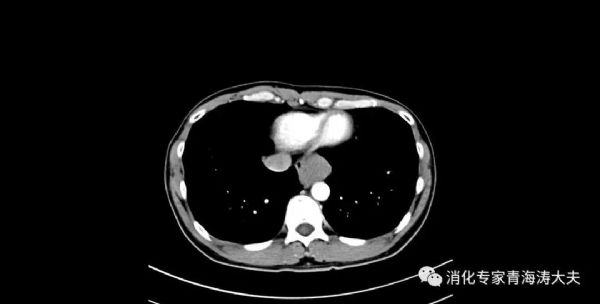
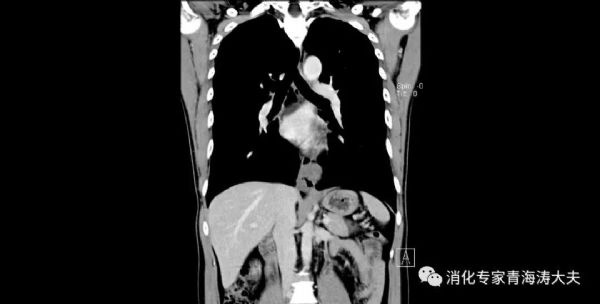
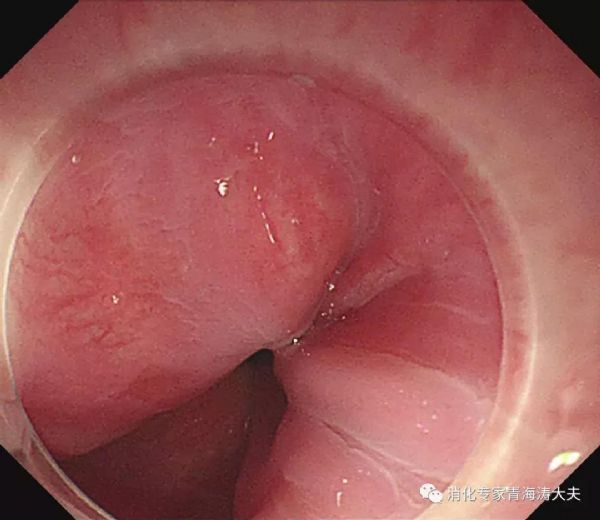
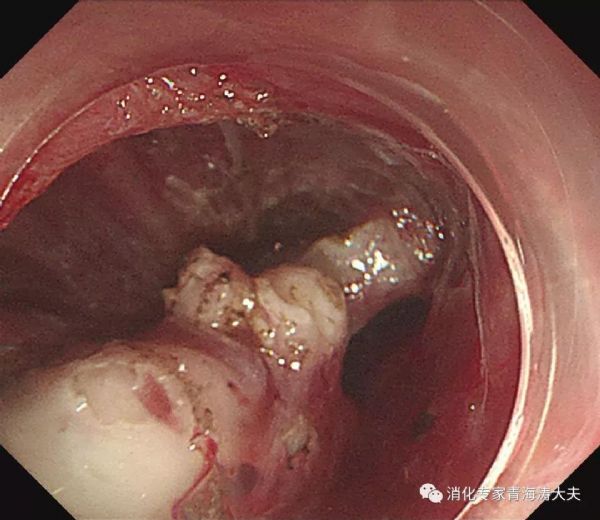
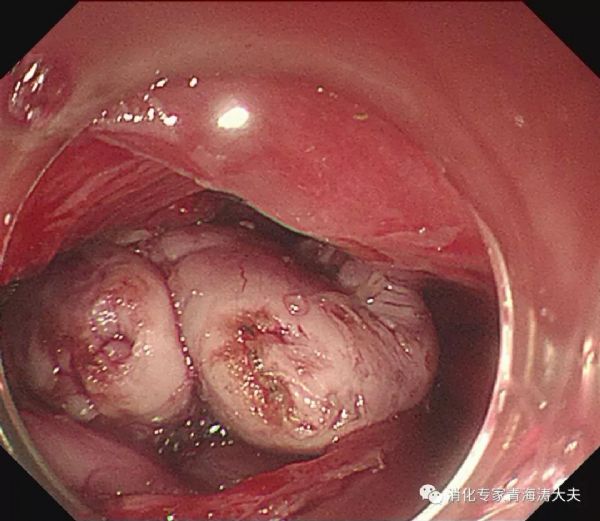
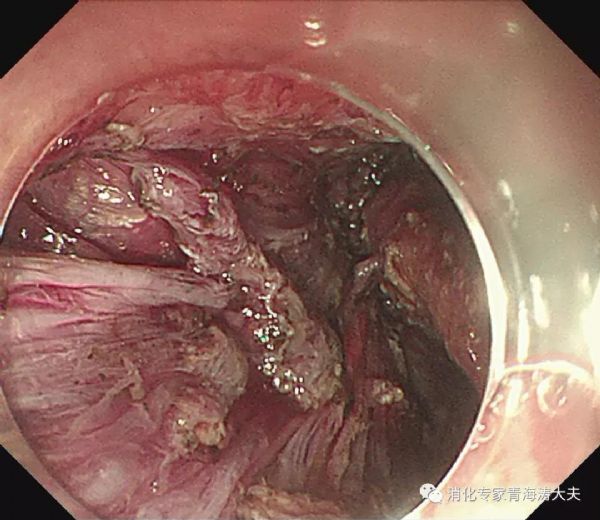
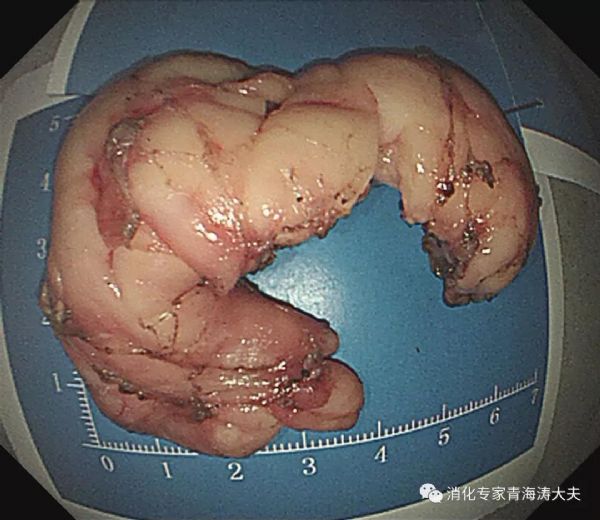
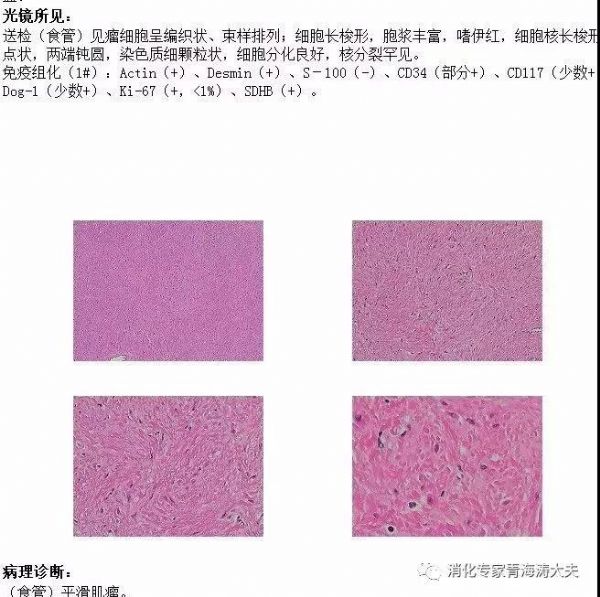
患者男,36岁,因发现食管肿物1月余入院,无胸痛、吞咽困难、消瘦等不适。术前评估考虑食管下段平滑肌瘤,行内镜下隧道技术切除病灶,病灶为环食管腔半周左右,大小10*4 cm。患者术后恢复良好,术后1周顺利出院,随访3月余至今无不适。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






















#内镜下切除#
78
#平滑肌#
95
#内镜#
95
#食管#
79
#平滑肌瘤#
75