J Urol:根治性前列腺切除术后新发储尿功能障碍是否常见?
2021-11-15 AlexYang MedSci原创
评估了男性新发储尿功能障碍的流行率、自然史和风险因素。
根治性前列腺切除术后,临床主诉的新发储尿症状可能与吻合口狭窄或压力性尿失禁有关。然而,有一部分男性会在没有吻合口狭窄或压力性尿失禁的情况下出现新的储尿症状。

近期,来自美国的研究人员在《J Uorl》杂志上发表文章,评估了男性新发储尿功能障碍的流行率、自然史和风险因素。

研究人员分析了2002-2019年之间,在RP之前排尿可控的且没有术后吻合口狭窄患者所填写的排尿症状调查表,并在RP后的第6、12、18和24个月,对新发储尿功能障碍进行了评估,评估结果为新发或恶化的尿急或尿频,并确定了其与患者和术前因素之间的关系。
储尿功能障碍定义为在感到有尿意时出现滴尿/漏尿的症状,难以推迟排尿,或在没有使用尿垫的情况下,在排尿结束后不到两小时就需要再次排尿,也意味着存在临床意义的压力性尿失禁。如果症状比基线时更严重,则认为是新发储尿功能障碍。排尿可控定义为无需尿垫。所有统计学分析均使用STATA15.0进行。
研究共有2619名患者最终纳入分析中。最初有34%的患者在6个月时报告出现新发储尿功能障碍,而在随后的第12个月随访中下降到26%。在第18个月和第24个月,比例分别为26%和23%。主要分析表明,微创手术(OR 1.36;95%CI 1.10, 1.68; p=0.005)与12个月时新发的储尿功能障碍有关,敏感性分析的结果类似。类似地,非白种人在两项分析中都与新发储尿功能障碍风险的增加有关,但在敏感性分析中没有达到显著性水平(主要分析:OR 1.29;95% CI 1.01, 1.65; P=0.041;敏感性分析:OR 1.24;95% CI 0.91, 1.68;P=0.2)。术后血肿在主要分析中达到了显著性水平,但在敏感性分析中没有达到显著性水平。
然而,这两项分析的置信区间并不排除有临床意义的结果(主要分析:OR 3.15;95% CI 1.04, 9.54;P=0.042;敏感性分析:OR 1.76; 95%CI 0.38,8.22;P=0.5)。最终,研究人员认为,微创手术和非白人种族与报告的症状恶化有关。术后血肿与症状恶化之间的关系还不太确定,但存在临床相关性(OR 3.15;95% CI 1.04, 9.54;P=0.042)。
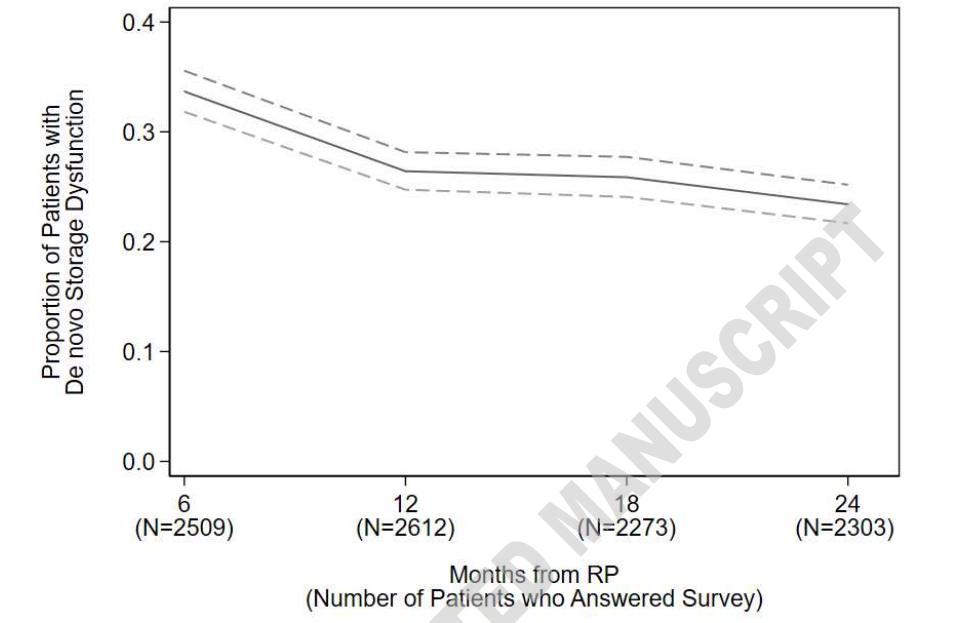
RP后新发储尿功能障碍患者的比例情况
综上所述,相当多的患者在RP之后会出现储尿功能障碍。接受过MIS手术的患者风险则会更高。因此,对有风险的患者应提供咨询,使其了解新发储尿功能障碍的发生率,并根据OAB指南进行早期治疗。
原始出处:
Kathleen M Kan , Amy L Tin , Gillian L Stearns et al. De Novo Urinary Storage Symptoms are Common after Radical Prostatectomy: Incidence, Natural History and Predictors. J Urol. Oct 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
70
#前列腺切除#
108
#功能障碍#
112
#根治#
71